Stroke and Transient Ischemic Attack (TIA)
What is it?
A stroke is a sudden brain injury caused by the interruption of blood flow to or sudden bleeding into a part of the brain. Broadly, there are two types of strokes: ischemic (85% of all strokes) and hemorrhagic (15% of all strokes). An ischemic stroke is caused by interruption in blood flow due to sudden blockage of a brain artery. A hemorrhagic stroke is caused by rupture of a brain artery leading to bleeding into the brain or into the spaces around the brain. Interruption of normal blood flow prevents the brain from receiving adequate nutrients (e.g., glucose and oxygen) necessary for survival. Bleeding into the brain causes compression and damage from swelling. Stroke results in permanent death of one region of the brain – it is a form of permanent brain damage.
The effects of a stroke depend on the location and severity of damage. Most commonly, a stroke is associated with weakness on one side of the body, difficulty with speech or understanding speech and loss of vision. Stroke can also result in cognitive difficulty (e.g., problems with speech, memory and concentration), loss of sensation or imbalance.
A transient ischemic attack (TIA) is the mildest form of ischemic stroke. It is a short-lived stroke lasting typically less than 30 minutes. A TIA is often a warning sign for a future major ischemic stroke.
A stroke can be a life-altering event, or a fatal event. In Canada, approximately one in six patients with stroke will die in the first 30 days. Stroke survivors may face great limitation in ability, necessitating alternate methods and assistance for carrying out everyday activities. It is common for older adults who have suffered stroke to require long-term care. However, almost every stroke survivor can recover some function. Treatments for acute ischemic stroke vary, but include: clot-busting drugs or advanced endovascular treatment in appropriately selected patients. In order to improve functional recovery, patients may be offered physiotherapy, occupational therapy, speech-language therapy and adjusted living (in the case of paralysis).
“An ounce of prevention is worth a pound of cure.” The best treatment for stroke is prevention. The likelihood of having a stroke can be greatly reduced by controlling blood pressure. Other modifiable risk factors for stroke include smoking, high alcohol intake, poor diet, high cholesterol and substance abuse. It is important to concurrently maximize physical activity, healthy diet and good sleeping habits.
Click to download the chart pack or infographic!
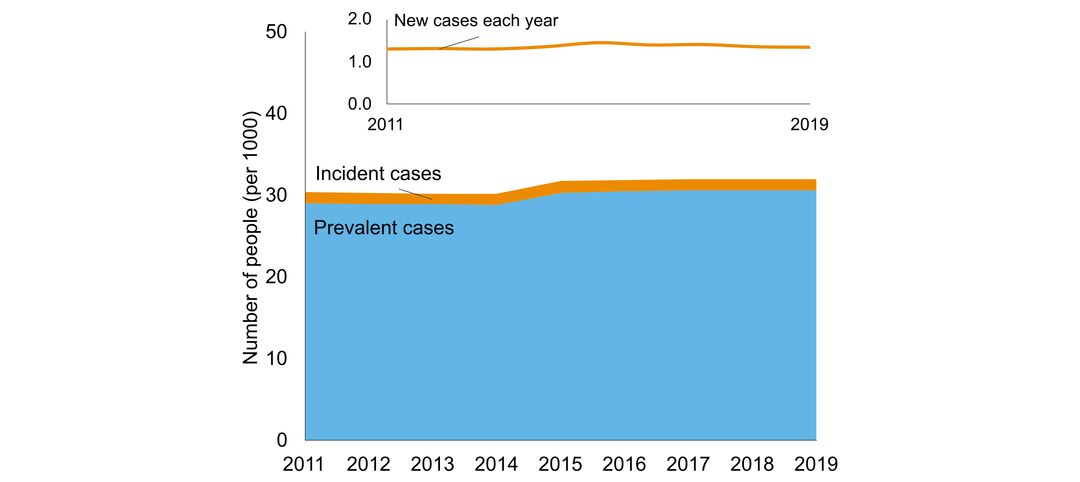
- number of people in Ontario with the disorder
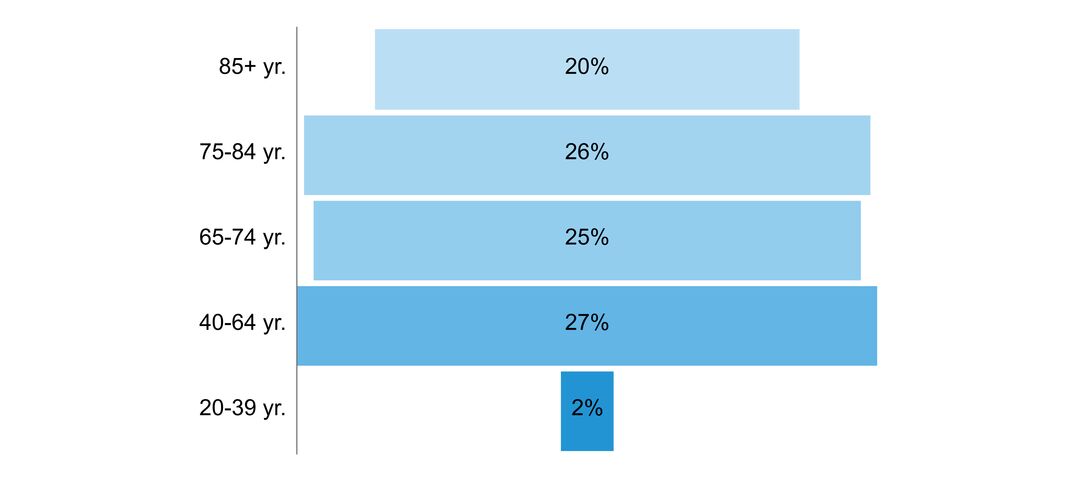
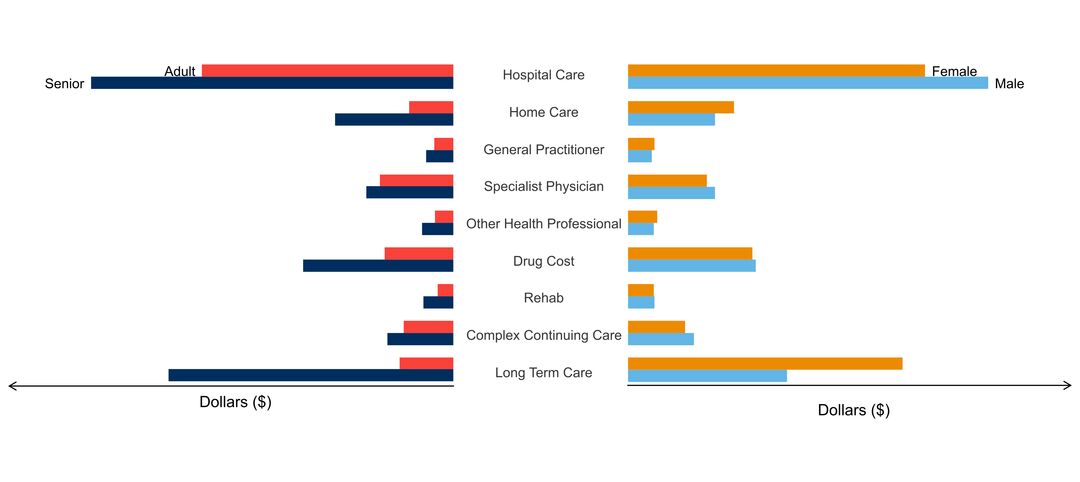
- age of people with the disorder
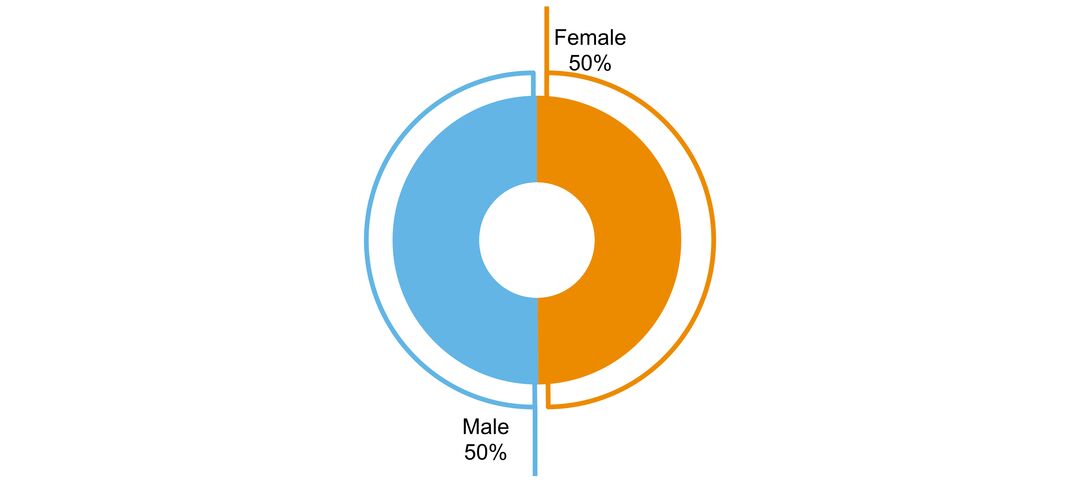
- sex ratio of people with the disorder
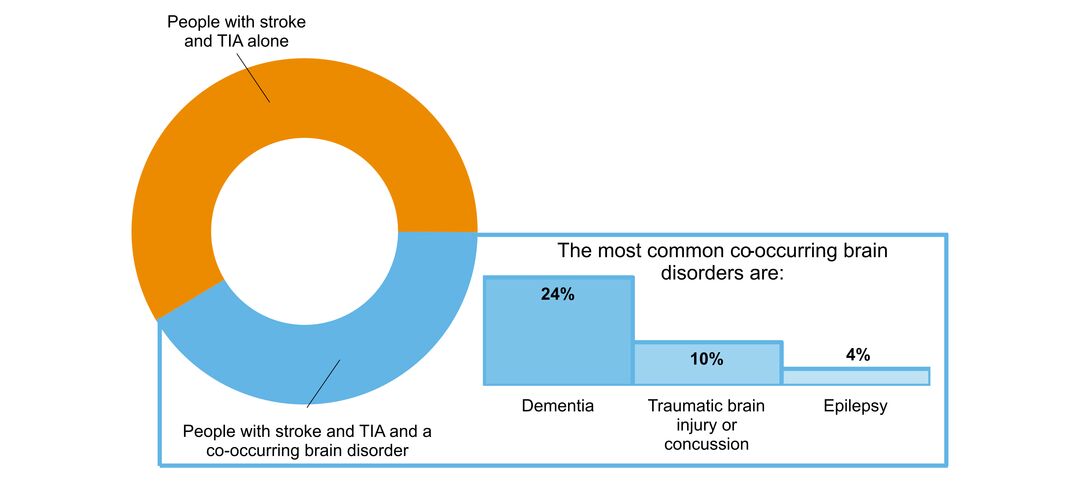
- what other brain disorders commonly co-occur
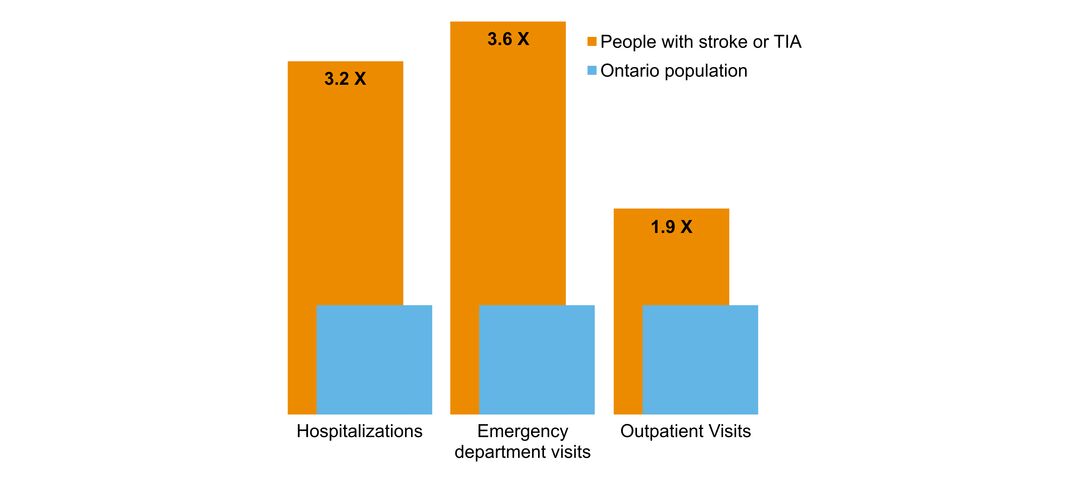
- overlap with mental health and addictions health system use
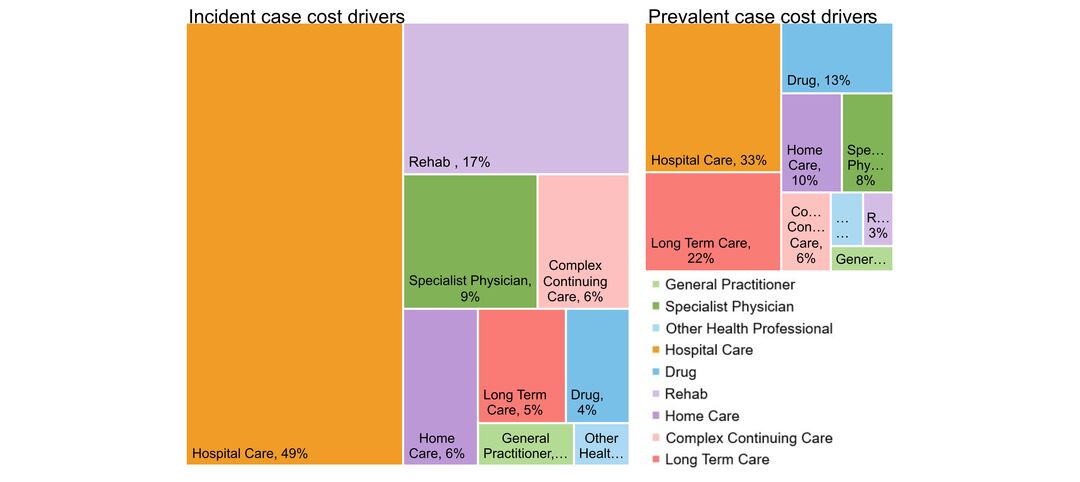
- costs & cost drivers associated with health system use