Schizophrenia
What is it?
Schizophrenia, including schizophrenia spectrum and schizoaffective disorders
Schizophrenia is a complex brain disorder that affects one’s ability to differentiate between what is and is not reality. Symptoms of schizophrenia are considered either positive or negative. The positive symptoms include the occurrence of delusions (false beliefs that are not amenable to change even in light of conflicting evidence, such as beliefs that one is going to be harmed, for example), hallucinations (elaborate sensory experiences such as hearing voices or seeing things that are not real), skewed perceptions (such as abnormalities in spatial awareness and sense of self) and disorganized thinking or behaviour. The negative symptoms affect aspects of cognition, expression of emotion, and motivation and include declines in attention, memory and deficits of normal emotional responses.
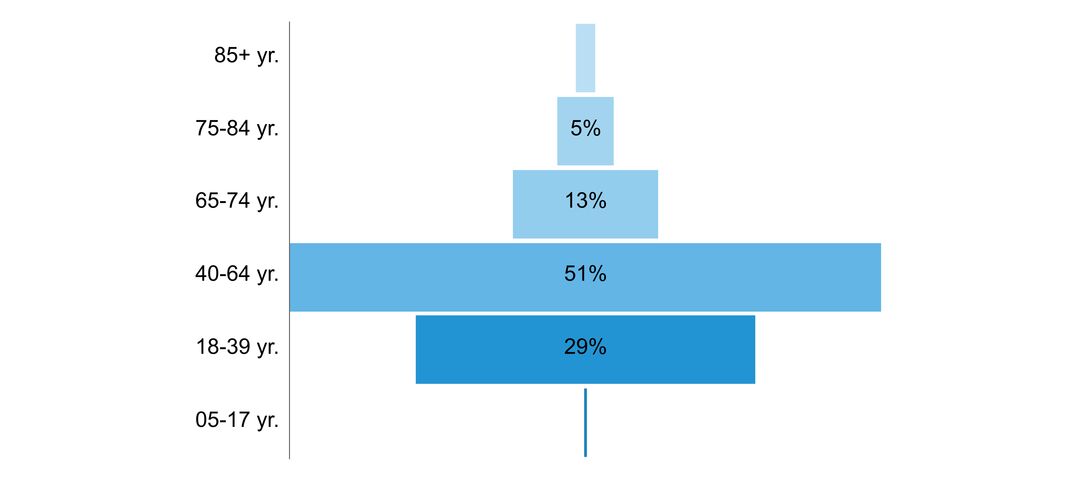
Schizophrenia typically presents in individuals between 16 and 30 years of age. Early on, schizophrenia may resemble a general anxiety or depression, with increasing difficulty with attention, relaxation, and sleep. A person may withdraw from social settings and usual activity, which can be upsetting and problematic for friends, family, and employers. When schizophrenia reaches an active, or psychotic, stage, the person may begin to behave erratically in response to having unusual beliefs or perceptions, or because his or her thoughts have become disorganized. Schizophrenia is both chronic and episodic in nature, worsening and improving by varying degrees. With each cycle, despite temporary improvement, residual symptoms increase and capacity for normal functioning typically declines. Many individuals with schizophrenia grow estranged from family and have difficulty holding consistent employment.
There is no known cure for schizophrenia, and the ebb and flow of the severity of symptoms makes treatment complex. Treatment involves using a combined approach of medication and psychosocial interventions. The positive symptoms can often be controlled with medication. The negative symptoms, however, are more persistent, difficult to treat, and often have the greatest impact on quality of life and disability.
Click to download the chart pack or infographic!
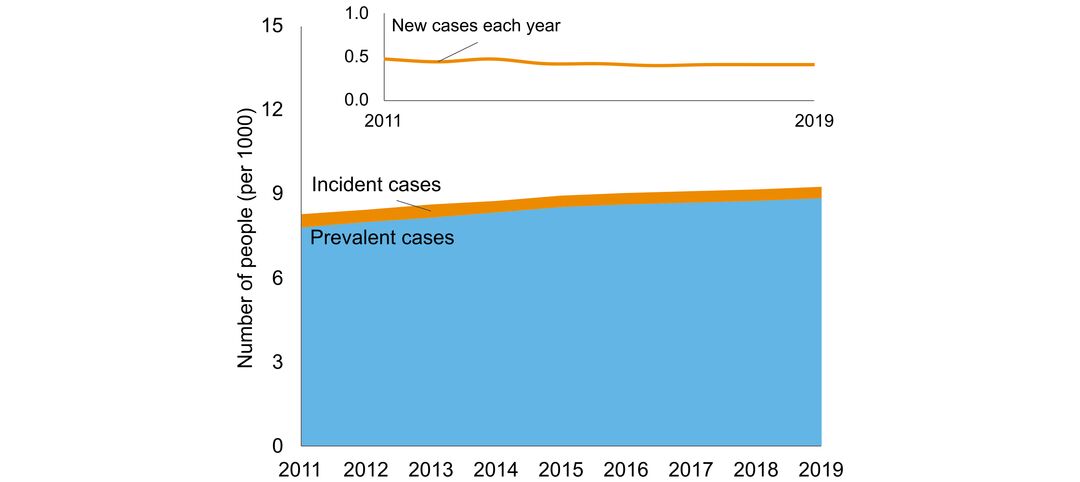
- number of people in Ontario with the disorder
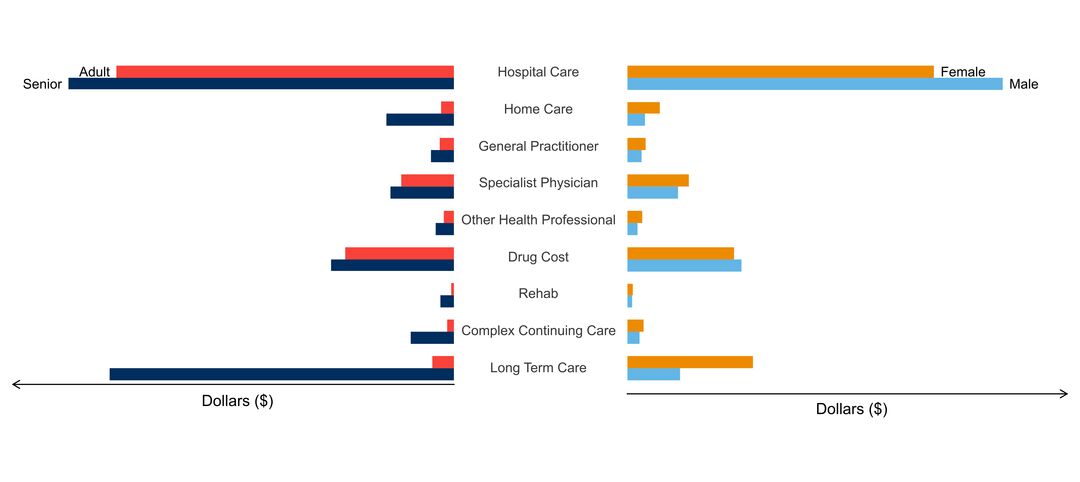
- age of people with the disorder
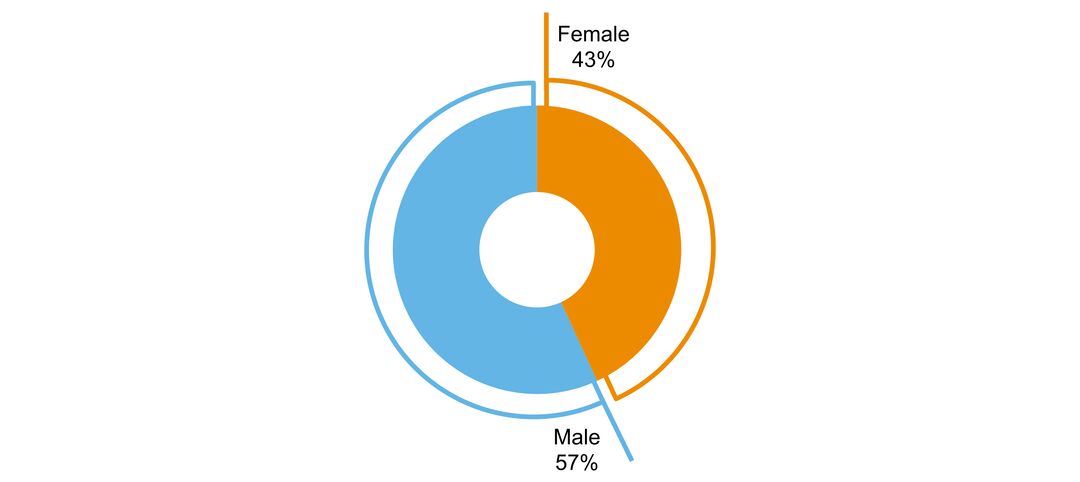
- sex ratio of people with the disorder
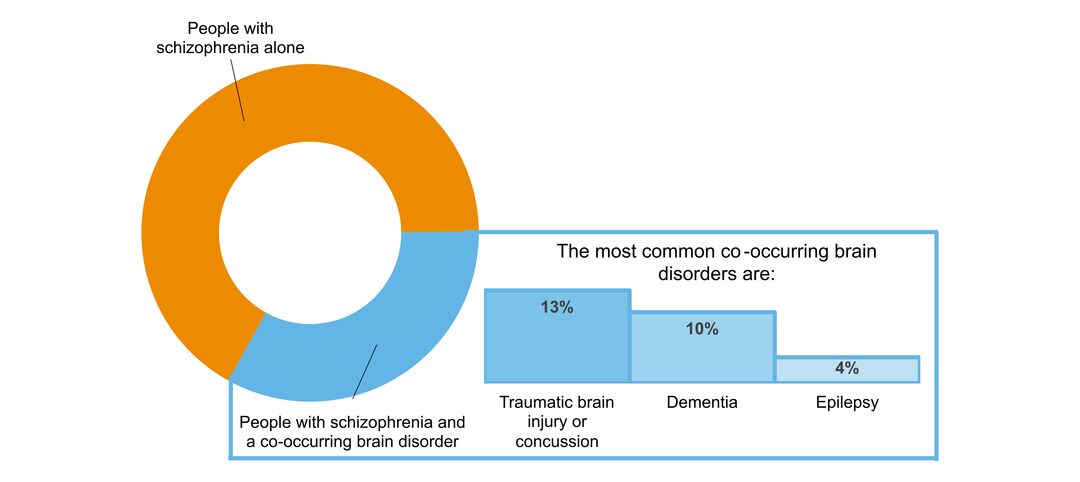
- what other brain disorders commonly co-occur
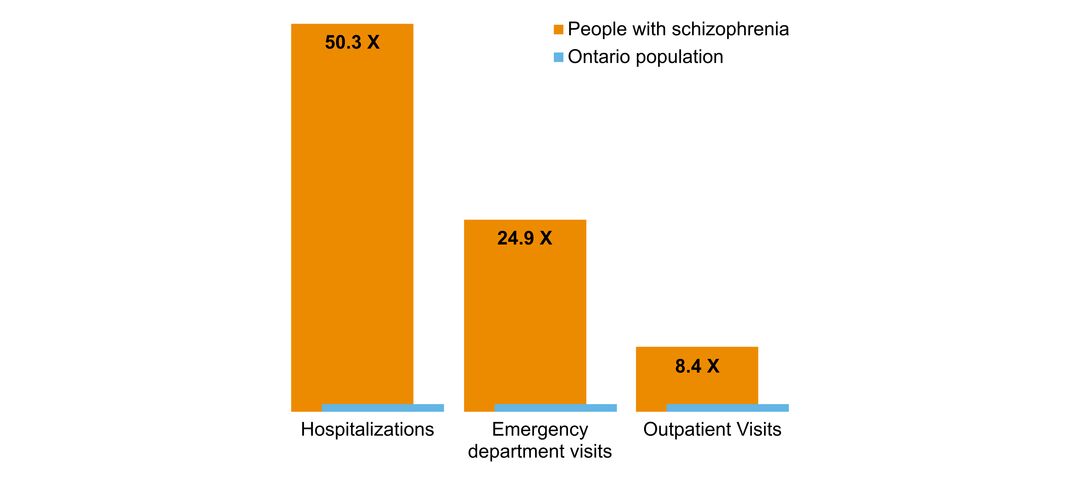
- overlap with mental health and addictions health system use
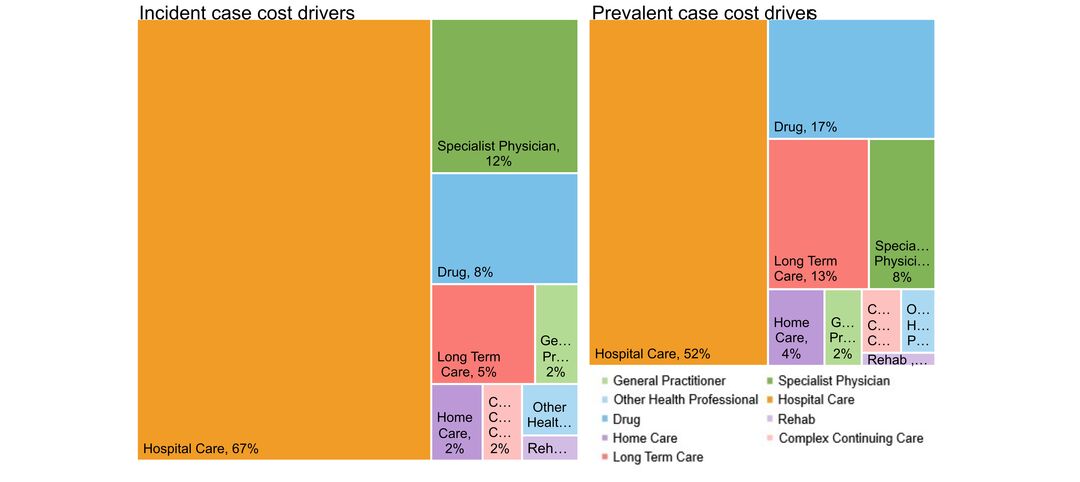
- costs & cost drivers associated with health system use