Brain Health in Ontario: Methodology
Methodology
To address the project’s objectives and provide comparable data consistently across brain disorders, a common approach was required. Years are reported by the fiscal year calendar. For example, the year 2011 represents the dates between April 1, 2011 – March 31, 2012.
Demographic Profile
A demographic profile was constructed for each brain disorder based on all individuals with that condition who were alive and residing in Ontario on April 1, 2019. Sex (male/female) and age groups in years are described. Summary statistics, including the mean (standard deviation) and median (interquartile range), were reported for age. Additionally, the number and proportion of individuals with a brain disorder were reported according to the following age groups: 0–4 years, 5–17 years, 18–39 years, 40–64 years, 65–74 years, 75–84 years and 85+ years. Specific age groups describing newborns (<1 year), children (0–17 years), adults (18/20/40–64 years) and older adults (65+ years) were also presented where applicable.
Prevalence
Prevalence for each brain disorder was determined on April 1 of each year from 2011 through 2019. Prevalence was calculated as the number of persons with a brain disorder on April 1 of a given year divided by the total mid-year population of Ontario measured as of July 1 of a given year. For brain disorders with age restrictions, the total population consisted only of individuals within the appropriate age range. For comparability between years, prevalence estimates were standardized by age and sex to the 2011 Census population for years 2011 – 2015, and 2015 Census population for year 2016 - 2019. Accrual of persons with brain disorders started on April 1, 1988 or April 1, 1991 depending on database availability, and was carried over to future years unless the persons died, left Ontario or lost health insurance eligibility.
Incidence
Incidence for each brain disorder was determined annually from 2011 to 2019. Incidence was calculated as the number of persons with a newly identified brain disorder accrued between April 1 and March 31 of the following year divided by the susceptible population. The susceptible population was counted as the total mid-year Ontario population minus those who already had the brain disorder. The ‘index date’ was used to define the date of incidence. As mentioned previously, this date may not be the true clinical diagnosis date of the disorder. For brain disorders with age restrictions, the susceptible population consisted only of individuals in the appropriate age range. The accrual period identified individuals with a pre-existing brain disorder so they would not be mistakenly counted as having a newly identified brain disorder in later years. For comparability between years, incidence was standardized by age and sex to the 2011 and 2015 Census population. The maximum follow-up date was March 31, 2020.
Costs Associated with Health System Use
There are many costs associated with health system use when a person receives care and treatment for their brain disorder or other coexisting health conditions. We provide a comparison of these direct costs paid by the Ontario Ministry of Health for a person with a brain disorder. These costs were calculated using Ontario health administrative data for a continuum of health care services categorized into seven types: complex continuing care, long-term care, home care services, hospital care, physician and other health care professional services covered by OHIP, prescription drugs and rehabilitation services. Costs included within the categories are described in Table 1 below.
We also provide and estimated cost comparison range for a person with a brain disorder compared to the average Ontarian. We calculated the mean 1-year cost of an incident case based on the 2019 incident case cohort by looking at the costs accrued up to 365 days from diagnosis date with a maximum follow-up date of March 31, 2020. The mean 1-year cost of a prevalent case was based on the 2019 prevalent case cohort using a one-year period, from April 1, 2019 to March 31, 2020. A general Ontario cohort was created, and costs calculated for a one-year period, from April 1, 2019 to March 31, 2020. While these data are not age and sex matched, cost comparisons were made between the disorder-specific relevant age groups of children (0–17 years), adults (18/20/40–64 years) and older adults (65+ years) described above.
Further description of costs calculation can be found in the original report Brain Disorders in Ontario: Prevalence, Incidence and Costs from Health Administrative Data published in 2015, found here.
Co-occurring brain disorders
Brain disorders do not always occur independently, but rather co-occur. To determine the degree to which certain brain disorders might co-occur, we identified the frequency of co-occurrence for each brain disorder by looking at the number of people within a given disorder cohort that also appear in one, two, or three or more brain disorder cohorts. We also looked at which brain disorders most often co-occur by identifying the proportion of individuals who appear in every other brain disorder cohort.
Mental Health and Addictions Service Use
Health service use for mental health and addictions related reasons was estimated using three Health Service Use Indicators related to rates of visits: (1) Rates of mental health and addictions–related outpatient visits, (2) Rates of mental health and addictions–related emergency department visits, and (3) Rates of mental health and addictions–related hospitalizations. Detailed definitions of visits can be found in the 2021 Mental Health and Addictions System Performance in Ontario Scorecard technical appendix, found here.
Health service use by persons with a brain disorder who were alive and eligible on April 1, 2019 were standardized to the 2015 census population and compared to the Ontario population alive and eligible April 1, 2019 (from Registered Persons Database).
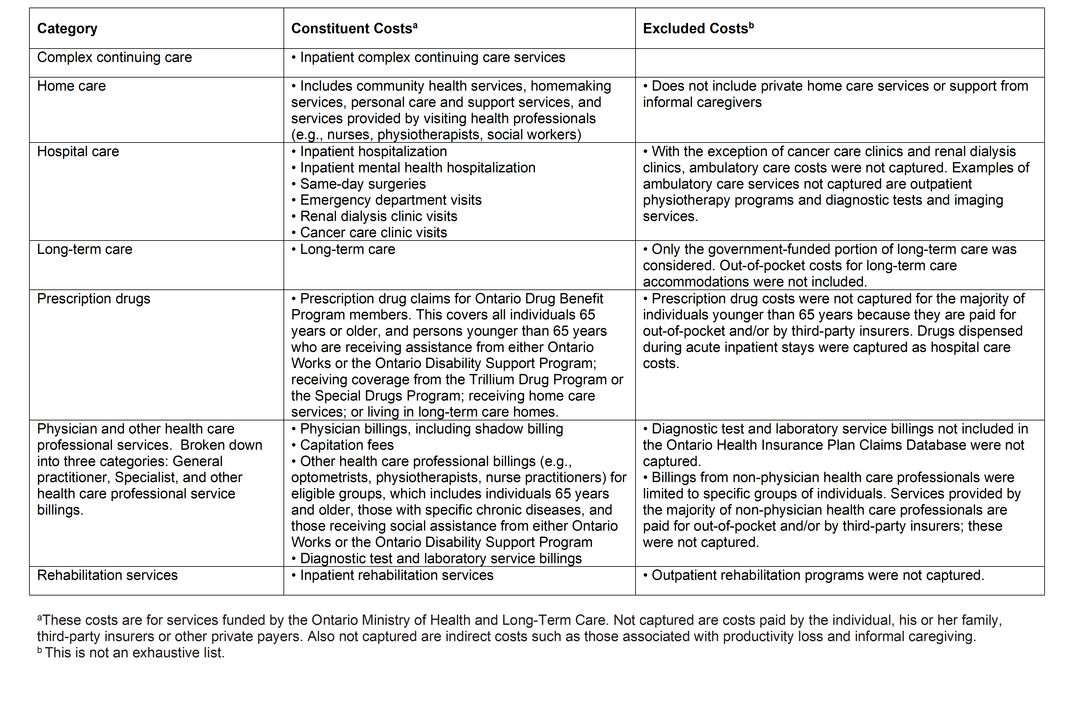
Table 1: Types of health care services and their constituent costs
General Considerations
Brain Disorder Algorithms
The algorithms used to identify individuals with each brain disorder are presented in the Codes and Conditions section. Each algorithm had been either (a) previously validated against another gold standard data source (such as an electronic medical record) or (b) previously developed or employed by experts with clinical and health administrative data experience. Health administrative data, with the exception of cancer registry records, do not contain a brain disorder diagnosis date. Rather, the data indicate a physician-specified reason for the health care service encounter or a physician-prescribed drug for reimbursement from the Ontario government. Thus, individuals identified by an algorithm can be thought of as being physician-diagnosed. However, it should be noted that although the reason stated in the data oftentimes agrees with an individual’s clinical diagnosis, in other situations, the reason provided is not an actual diagnosis. Rather, the stated reason could be a clinical suspicion of the disorder or a negative test result. It is also common for an individual to present with several health problems, but not have all of them captured through diagnostic codes for a specific health encounter. These difficulties are handled with algorithms featuring time sequencing and repetition, which improves the identification of true positives and true negatives; however, the algorithms are not perfect.
Inclusion and Exclusion Criteria
For each brain disorder, the ‘index date’ was the earliest health system encounter with a relevant diagnostic code, drug code or entry in the cancer registry. For algorithms requiring a series of health system encounters of the same type (e.g., the dementia algorithm requiring three physician claims records at least 30 days apart in a two-year period), the date of the most recent encounter in that series was used to determine the index date. Individuals’ age and sex had to be known on the index date in order for them to be included. In addition, individuals had to be Ontario residents and covered by Ontario health insurance at the time. The Ontario Health Insurance Plan’s Registered Persons Database was used to confirm these inclusion criteria. Persons residing in Ontario but not eligible for provincial health insurance coverage (including refugee claimants, tourists and international students or individuals covered by other programs, such as Canadian Armed Forces personnel and federal inmates) were not counted. Further, some brain disorder algorithms had age restrictions in order to improve algorithm performance or because identification of some disorders is not feasible in younger populations. Individuals with multiple brain disorders are eligible to be counted as long as they meet the criteria (i.e., the conditions are not mutually exclusive).
Co-occurring brain disorders
The methodology used to identify co-occurrence among brain disorders is only possible amongst the disorders assessed in this project. Notably, several major brain disorders are missing, including but not limited to neurodevelopmental disorders, ADHD, anxiety, depression, mood disorders, and substance use disorders.
To estimate the co-occurrence of mental health issues and substance use among people with a brain disorder, we compared visit rates for these reasons between people with a brain disorder and the 2015 Ontario census population. Visit reasons in this analysis include: substance-related and addictive disorders, schizophrenia spectrum and other psychotic disorders, mood disorders, anxiety disorders, deliberate self-harm, trauma and stressor-related disorders, obsessive-compulsive disorder and related disorders, and personality disorders.
Disorder specific considerations
Cerebral palsy
Cerebral palsy is a developmental disorder that most commonly occurs during pregnancy, the prevalence for children 5 years and younger was estimated instead of incidence or newborn prevalence because diagnosis can be delayed or go unrecognized until 5 years of age.
Spina Bifida
Because spina bifida is a congenital developmental disorder, live birth prevalence was estimated instead of incidence. Yearly live birth prevalence was calculated by dividing the number of individuals born with spina bifida by the newborn population of that year.
Limitations
The data collected for the purposes of this project are not collected for research purposes and are therefore not without limitations.
The availability, reliability and validity of diagnoses and drug claims in the data are subject to administrative rules governing service provision, as well as financial incentives associated with payment for services. Not only must an individual make health system contact, but a diagnosis or drug therapy related to his or her brain disorder must also be recorded. This requirement will introduce bias into estimates as healthier individuals with less health system contact or those with less severe disorders or at earlier stages may be missed. With the exception of cancer, information on disease severity, stage or subtype is not typically available in health administrative data, and date of onset is difficult to calculate. In addition to potentially underestimating prevalence among individuals with less severe brain disorders, the lack of refinement in diagnostic codes (i.e., the number of ICD digits available across jurisdictions) typically precludes the identification of disorder subtype. Currently, there is a wide variety of algorithms in use across Canada, and there is variability in the databases that are included, the time periods for brain disorder accrual, the number of encounters required and the temporal sequence of those claims. Consistency of measurement across jurisdictions can be challenging given that different provinces have different health administrative data holdings and different rules/incentives/restrictions for health insurance administration, payment and coverage. Despite the above caveats, the estimates of prevalence and incidence included in this project are a starting point for establishing regular measurement and reporting on brain disorders across the province over time.
There are two important caveats regarding the cost calculations data. First, the costs associated with health system use include all health system contact, not only services related to the care or treatment of an individual brain disorder. For example, if an individual had surgery for a heart condition or received a drug therapy for arthritis in the relevant time period, these costs were counted in the analyses. In other words, it is not possible to draw conclusions regarding the specific costs attributable to a given brain disorder from the data presented in this project. Second, this project does not capture all possible costs associated with brain disorders. Specifically, the project only captures costs from the perspective of the Ontario Ministry of Health (MOH); it does not capture services that are paid for privately (i.e., payments to third-party insurance companies and other out-of-pocket payments for services) by an individual or his or her family, services paid for by other provincial ministries, or informal costs, such as when family members or friends serve as caregivers. The most significant missing attributable costs are those associated with ambulatory care in acute care hospitals. Examples of missing ambulatory care services include specialist clinics, imaging clinics and outpatient rehabilitation clinics. Examples of the sorts of costs that are not included in this project because they are not considered from the perspective of the MOH are private home care, over-the-counter drugs and health products, and equipment and supplies to support mobility. Although these are important components of the overall cost profile of individuals with brain disorders, it is simply not feasible to capture such costs using existing health administrative data. An important example of these data limitations is the relative absence of prescription drug costs for the majority of individuals younger than 65 years, as these costs are typically covered by third-party insurers. This exception is important to note when considering the overall cost analyses and the breakdown of costs by sector as there will be certain brain disorders, such as epilepsy, where drugs are an important component of care in younger populations but not captured in the project’s cost calculations. For these brain disorders, the project presents an accurate description of costs to the Ontario Ministry of Health but not to society more broadly. Prescription drug data were available for selected younger individuals receiving assistance from Ontario Works (a social assistance program for those in temporary financial need) or the Ontario Disability Support Program (a social assistance program for individuals with disabilities who are in financial need); receiving coverage from the Trillium Drug Program or the Special Drugs Program; receiving home care services; or living in long-term care homes.
