Spina Bifida
What is it?
Spina bifida is a neurological disorder occurring as a result of impaired growth of the neural tube during embryonic development (neural tube is the term for the brain and spinal cord during the embryonic phase of development); this results in varying degrees of damage to the spinal cord and brain. The exact cause of spina bifida is not currently known.
Children born with spina bifida can have a lesion on their spinal cord, making it vulnerable to injury and resulting in significant irreparable damage. Similar to spinal cord injury, the extent of damage from the lesion depends on where it occurs on the spinal cord, with higher lesions resulting in more damage. Three types of spina bifida are most common and range in severity. Myelomeningocele is the most severe where the spinal cord and the meninges (its protective covering) both push through the open part of the spine. Meningocele describes the situation when only the meninges push through the opening and typically no nerve damage occurs, although individuals may have minor disabilities. Spina bifida occulta is also referred to as ‘hidden’ because the protrusion is covered by skin and does not cause harm.
There is no known cure for spina bifida. However, some forms of spina bifida are treatable with surgery soon after birth in order to prevent infection and further damage to the spinal cord. Fetal surgery prior to birth is also available for some forms of spina bifida. Individuals with spina bifida may require devices to help with walking, and surgery may also be necessary to help manage ongoing complications.
Click to download the chart pack or infographic!
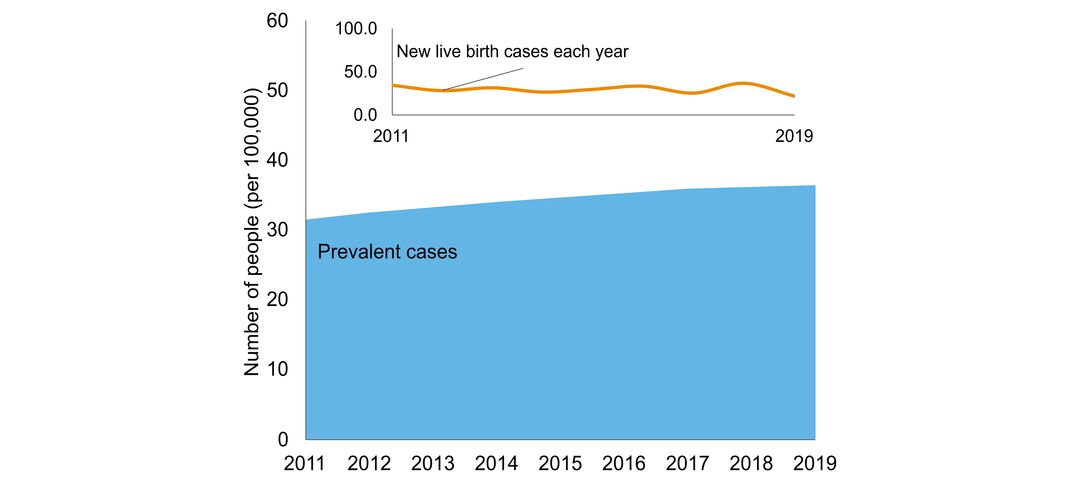
- number of people in Ontario with the disorder
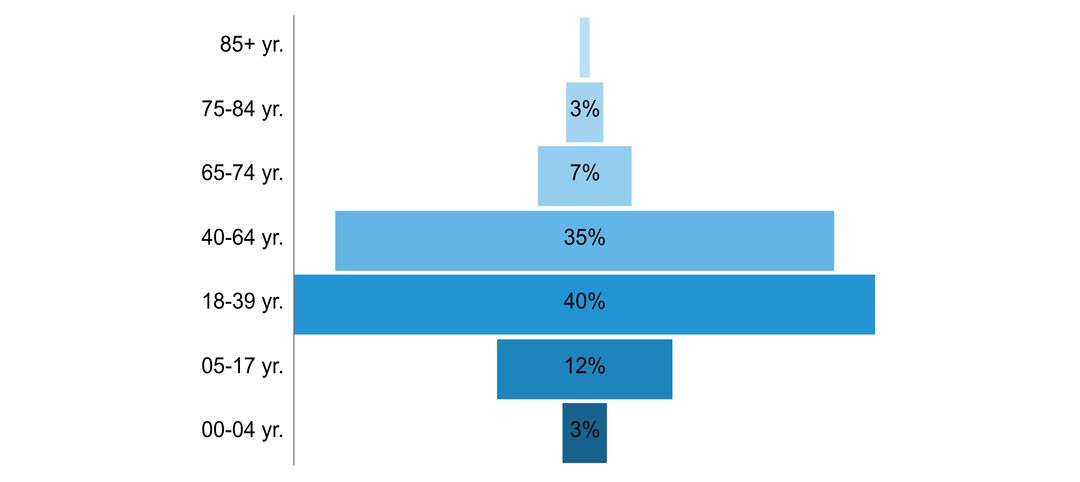
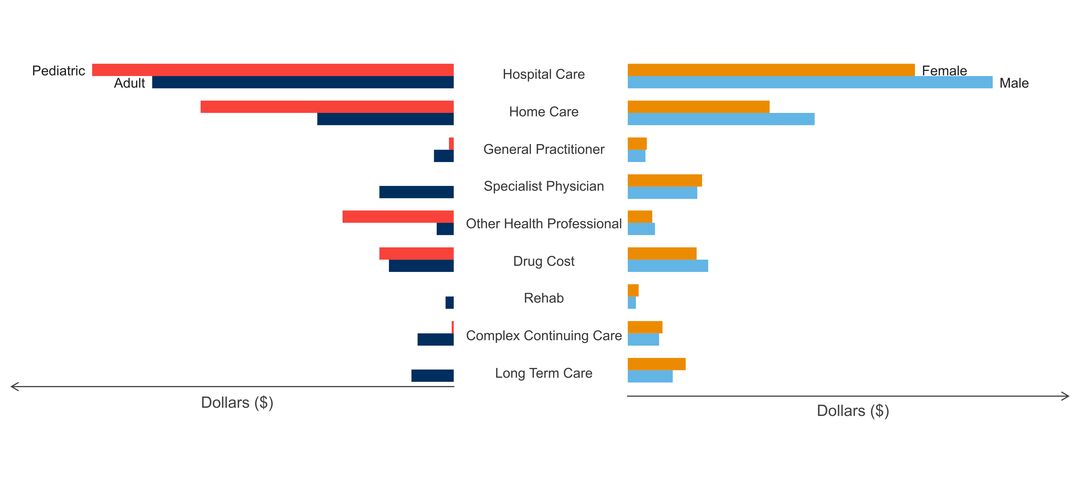
- age of people with the disorder
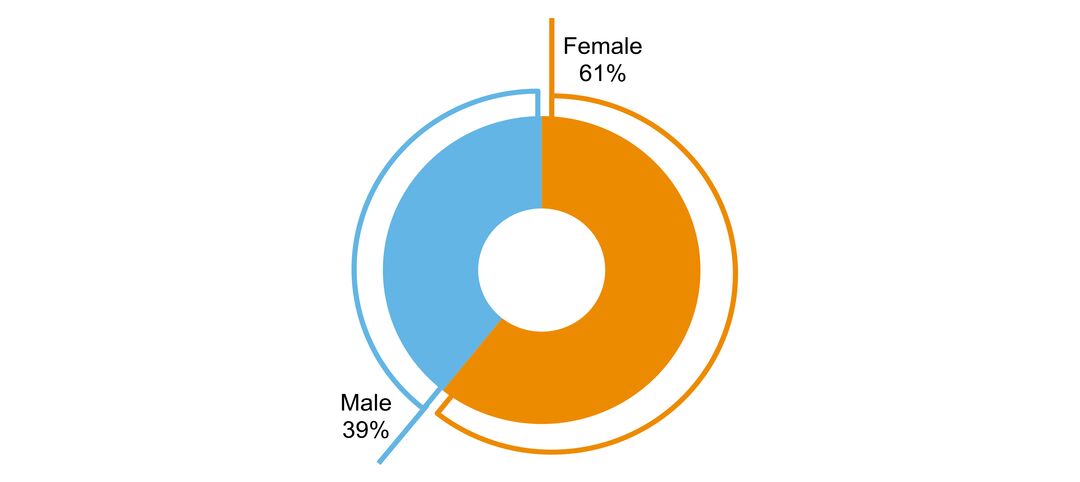
- sex ratio of people with the disorder
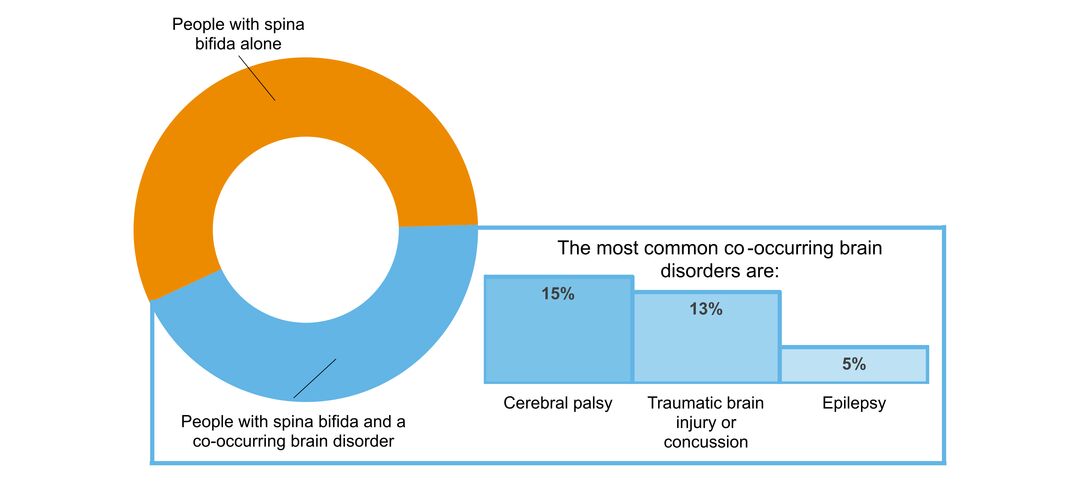
- what other brain disorders commonly co-occur
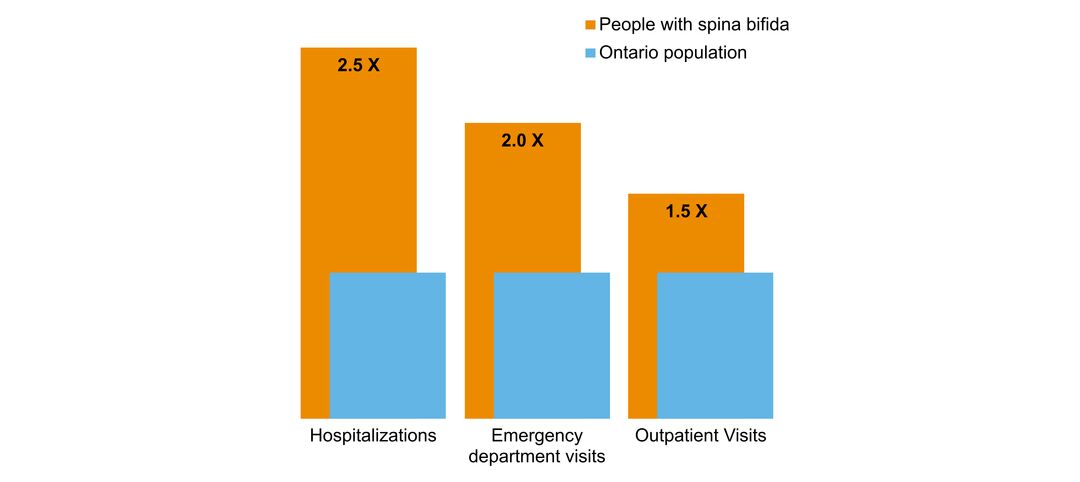
- overlap with mental health and addictions health system use
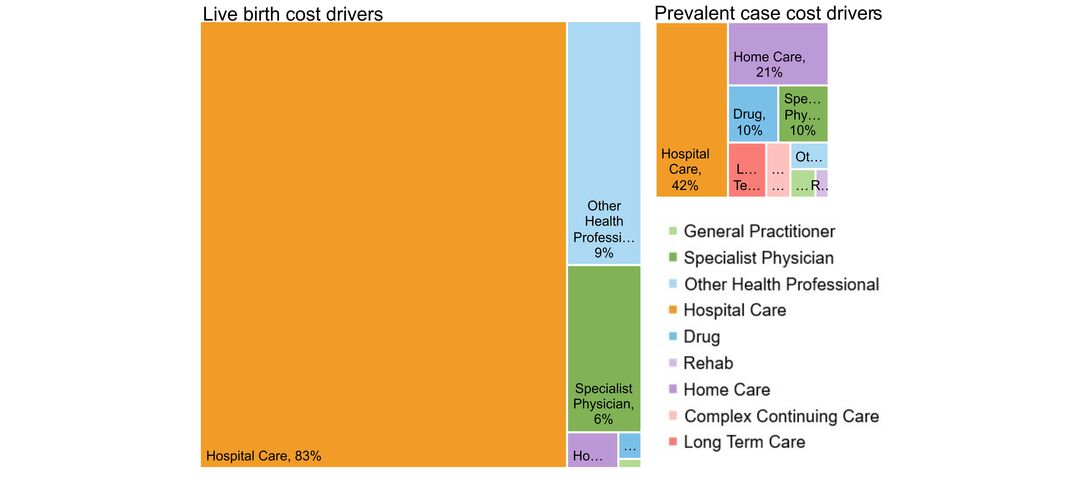
- costs & cost drivers associated with health system use