Multiple Sclerosis
What is it?
Multiple sclerosis is considered to be an immune-mediated disease of the central nervous system. The disease affects the protective covering of the nerve (myelin) and damages the nerve fibers (axons). The result may be a wide variety of symptoms, depending on what parts of the central nervous system are affected.
The cause of multiple sclerosis remains unknown. However, it is considered to be a complex disease in which one or more environmental factors act together in a genetically susceptible individual to cause disease. The genetic factors most consistently associated with multiple sclerosis involve the HLE allele. Environmental factors of particular interest include Epstein-Barr virus infection, vitamin D insufficiency, smoking and obesity.
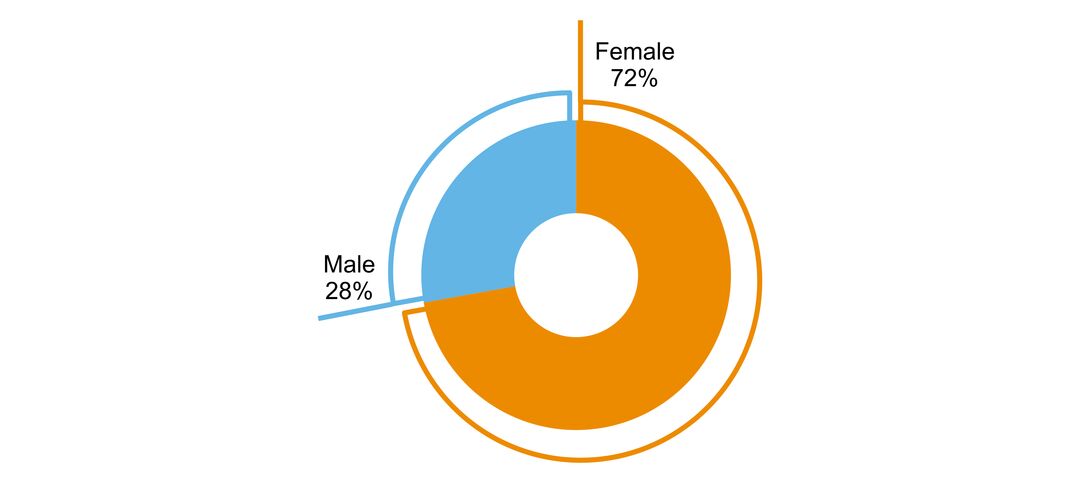
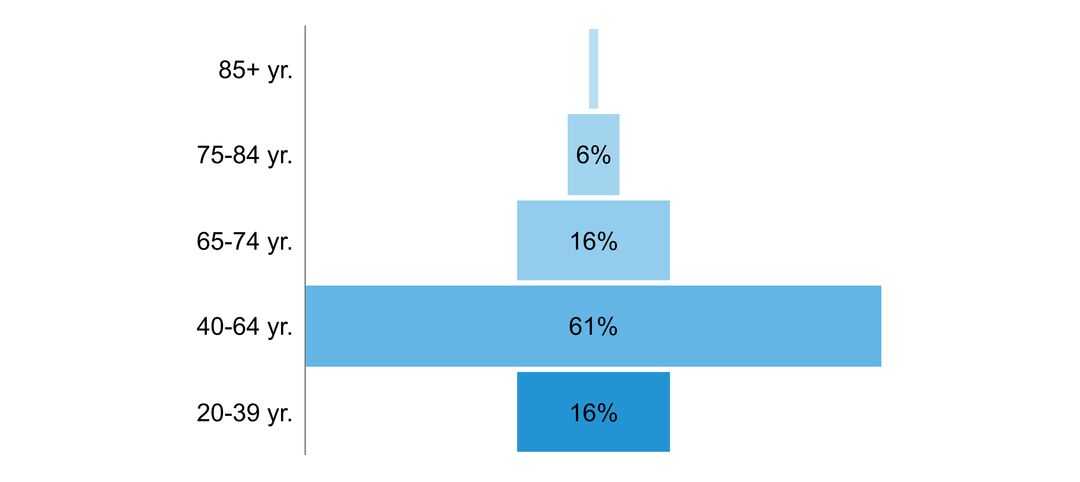
Multiple sclerosis is the most common non-traumatic cause of disability in young adults. Most affected individuals present with symptoms between the ages of 20 and 40 years. Women are affected nearly three times as often as men. The disease is variable from one person to another, and the ability to predict outcomes is limited. Most affected individuals present with an initially relapsing-remitting course. Symptoms are stable between relapses, but most individuals will develop gradual disability progression (secondary progressive multiple sclerosis). About 15% of persons have a gradual progression of disability from onset (primary progressive multiple sclerosis). Ultimately, most patients experience a constellation of symptoms, including weakness, sensory symptoms, bowel and bladder dysfunction, fatigue, spasticity, pain and cognitive impairment. Multiple sclerosis adversely affects employment and social relationships, and burdens the affected individual, their family, the health care system and society. Quality of life is lower in persons with multiple sclerosis compared to the general population and persons with other chronic diseases.
Treatment involves treatment of acute relapses, use of disease-modifying therapies and chronic symptom management. While there have been major advancements in disease-modifying medications that reduce the risk of relapses and delay progression in relapsing forms of multiple sclerosis, there are currently no approved disease-modifying therapies for primary progressive multiple sclerosis.
Click to download the chart pack or infographic!
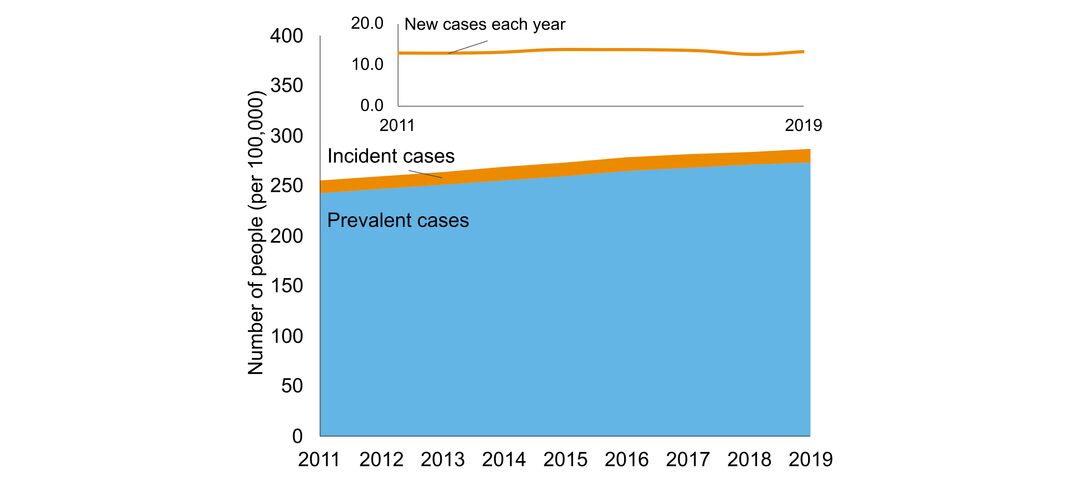
- number of people in Ontario with the disorder
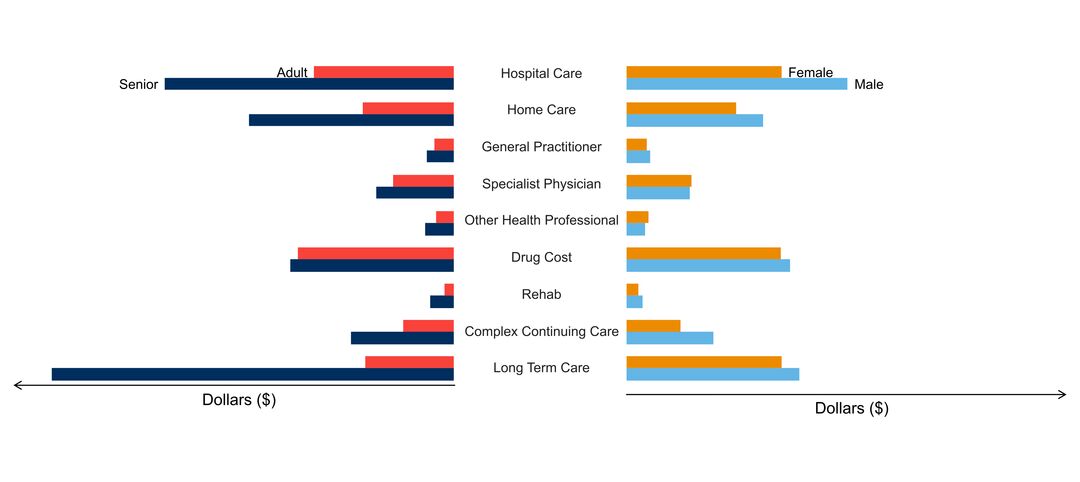
- age of people with the disorder
- sex ratio of people with the disorder
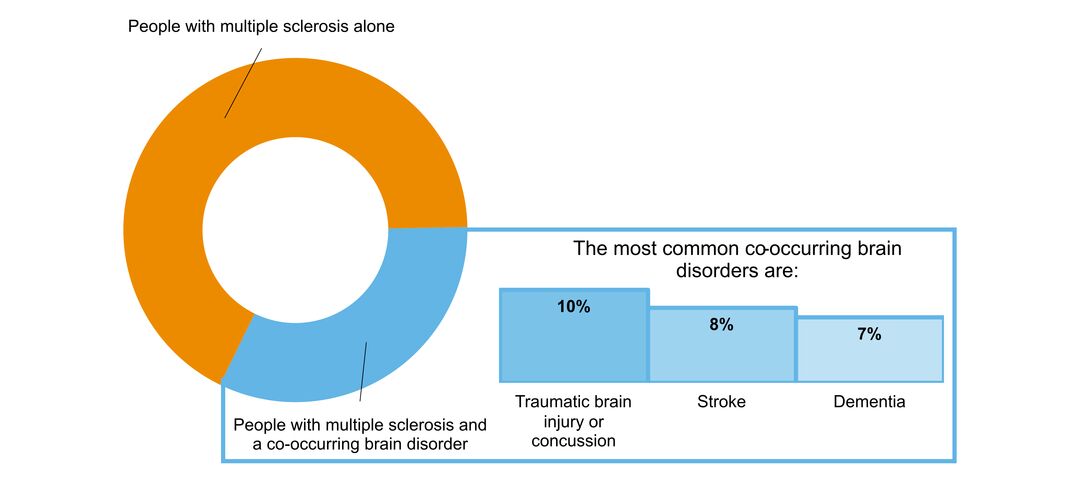
- what other brain disorders commonly co-occur
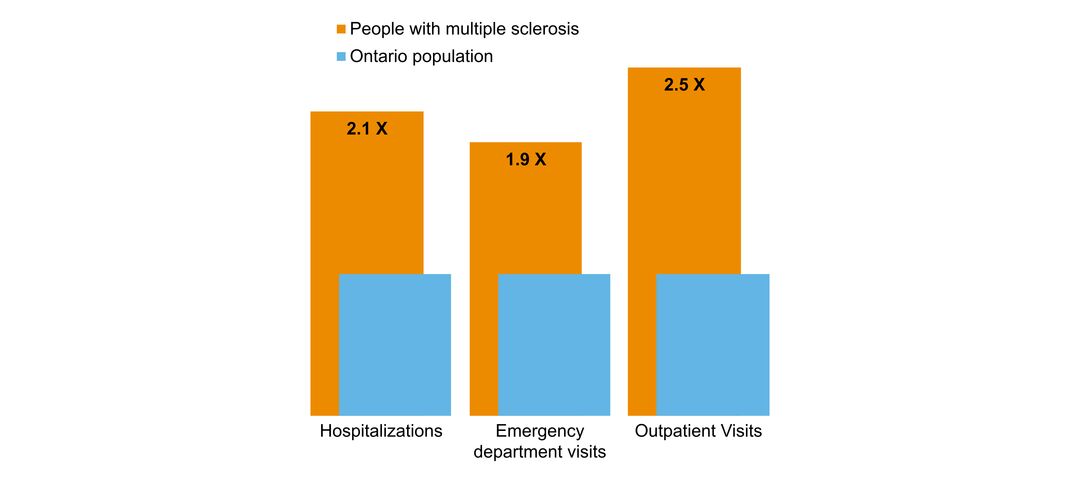
- overlap with mental health and addictions health system use
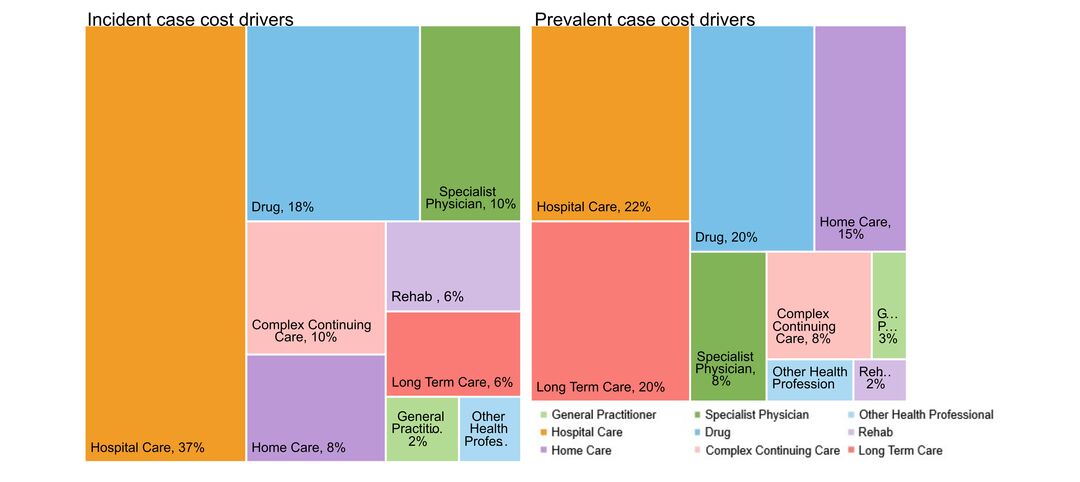
- costs & cost drivers associated with health system use