Parkinsonism
What is it?
Parkinsonism (including Parkinson’s disease)
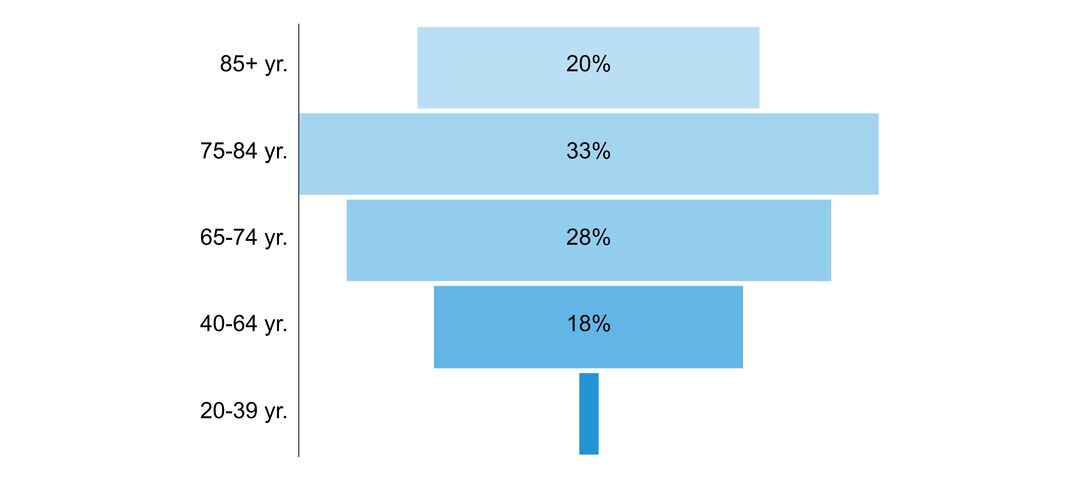
Parkinsonism describes a cluster of symptoms including tremor, rigidity (stiffness), akinesia or bradykinesia (loss or slowness of voluntary movement) and postural instability (tendency to fall). Parkinsonism typically affects persons aged 50 years and older. The most common cause of parkinsonism is Parkinson’s disease. Other causes include other brain disorders, toxins, medications and inherited disorders. These various causes lead to parkinsonism through changes in a region of the brain called the basal ganglia. Among persons with Parkinson’s disease, there is evidence of a loss of dopamine-producing neurons in the substantia nigra part of the basal ganglia.
An individual with parkinsonism will experience difficulty with initiation and completion of movement, with fine motor skills and with walking. Other difficulties include effects on swallowing, volume of voice, blinking and initiation of spontaneous facial expressions. Parkinsonism also causes unintentional movement in the form of tremor, which in the hand can resemble the rolling of a pill or small object when the hand is at rest. Symptoms not related to motor function include cognitive impairment, mood disturbance including depression, anxiety and apathy, constipation and bladder disturbance, pain related to rigidity, and disordered sleep – all of which greatly hamper quality of life. In patients with onset before the age of 65, parkinsonism may lead to premature retirement or necessitate disability leave. Parkinsonism also impairs the ability to communicate and interact with the surrounding environment, which often instills a sense of isolation among affected persons. Dopamine replacement medications can help some of the symptoms of parkinsonism, especially in Parkinson’s disease, but these effects are usually transient and there are no cures.
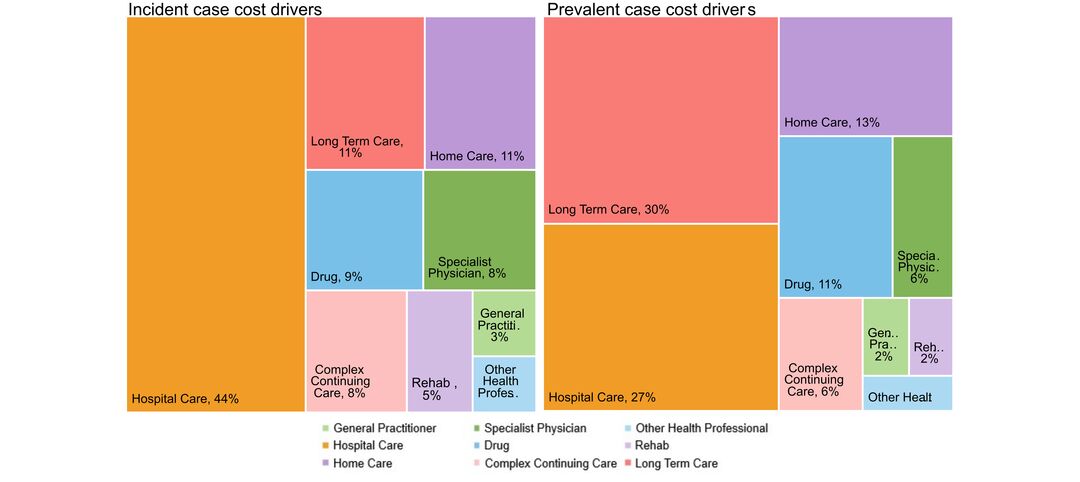
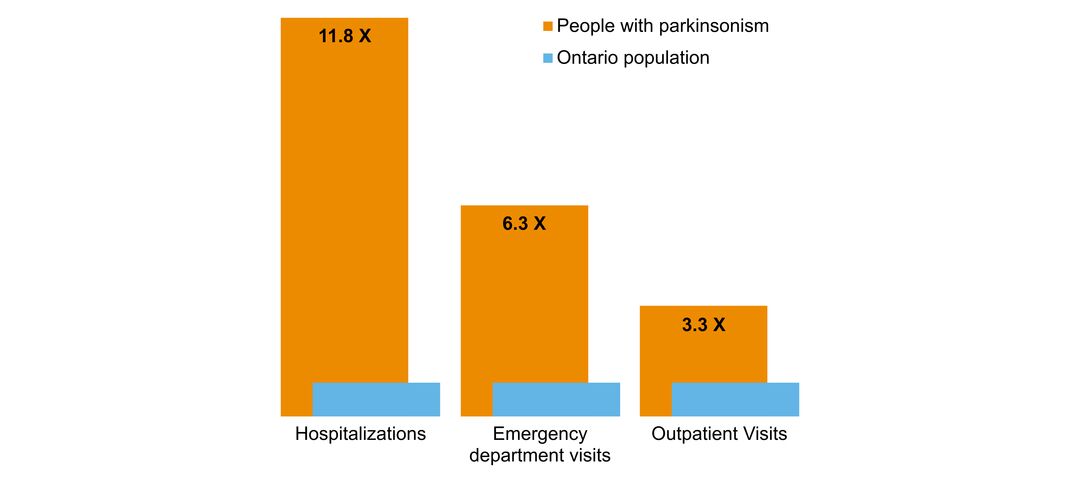
Many symptoms of parkinsonism cause complications leading to hospitalization – among them, pneumonia and other infections and fall-related injuries. Further, individuals with parkinsonism may develop significant cognitive impairment and psychiatric changes including hallucinations leading to nursing home placement. Persons with advanced parkinsonism require caregiver help and may become completely dependent for all activities of self-care.
Click to download the chart pack or infographic!
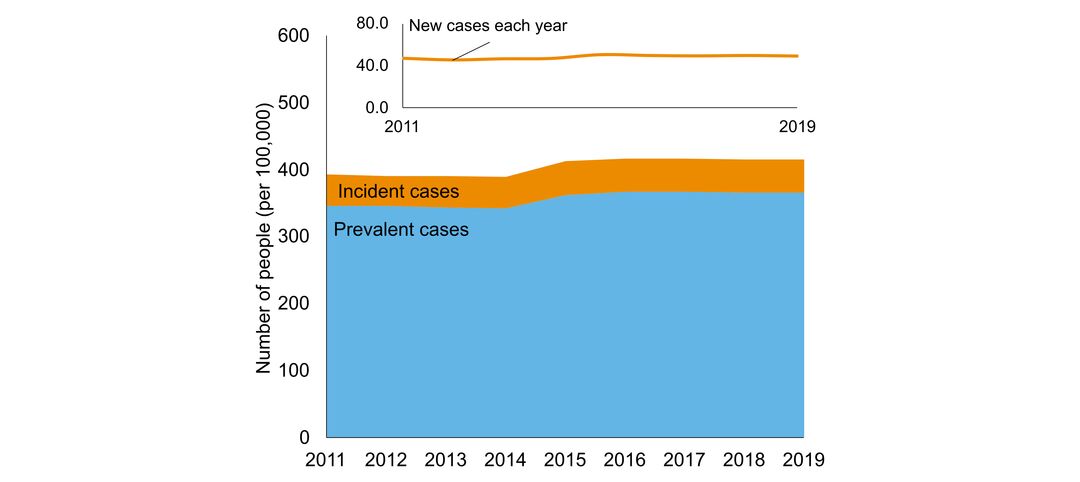
- number of people in Ontario with the disorder
- age of people with the disorder
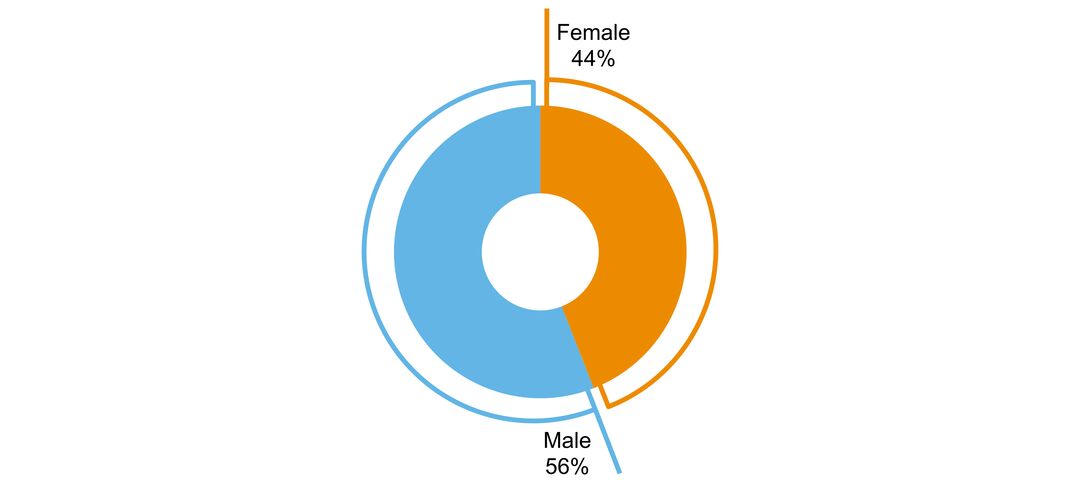
- sex ratio of people with the disorder
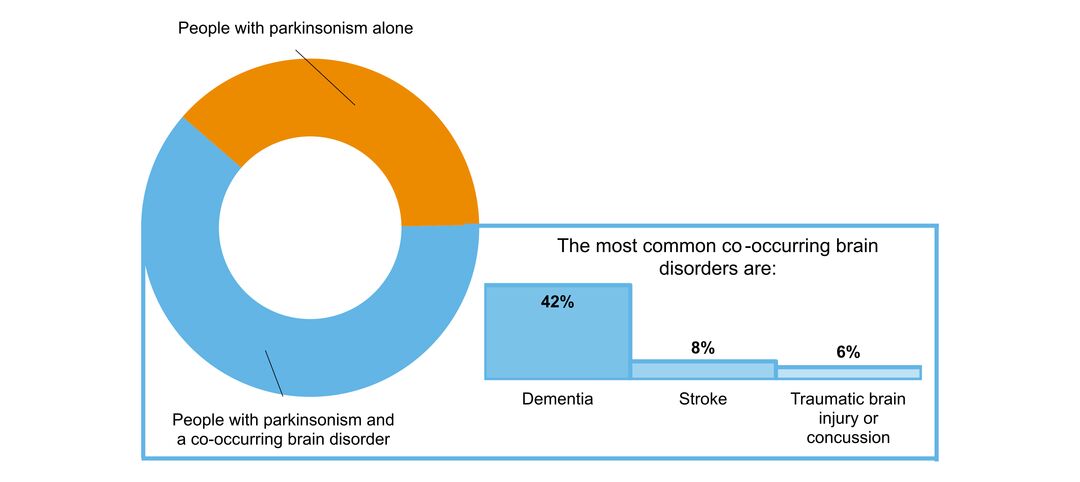
- what other brain disorders commonly co-occur
- overlap with mental health and addictions health system use
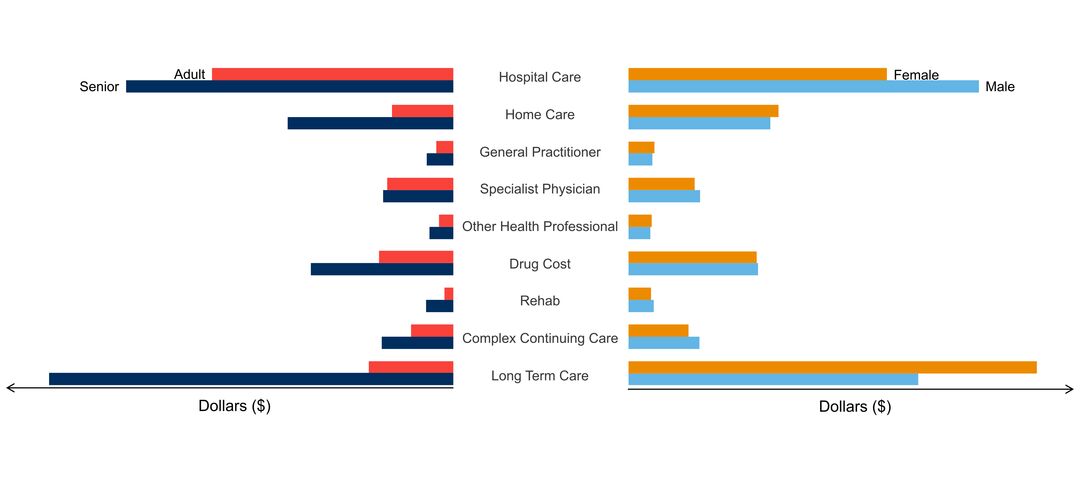
- costs & cost drivers associated with health system use