Epilepsy
What is it?
Epilepsy, sometimes referred to as a “seizure disorder,” is a common brain disorder characterized by recurrent seizures. A seizure is a burst of uncontrolled electrical activity in the brain which, depending on the part of the brain involved, can cause a disruption in sensation or behaviour. Since many different brain regions may be involved in the development and spreading of seizures, the experience and clinical presentation of epilepsy can take various forms – from feeling anxious to experiencing tonic-clonic seizures, which are characterized by loss of consciousness and severe muscle contractions. Seizures can be provoked by a number of factors including chemical imbalance, head trauma, and illness, while other factors such as stress and fatigue can trigger seizures. Susceptibility to seizures varies between individuals and is also influenced by genetic and environmental factors.
While seizures are often unpredictable, some individuals retain awareness at the onset of, or even throughout, their seizure. Manifestations at the beginning of a seizure, such as a sense of déjà vu, a distortion of reality, a foul smell or a “rising sensation” (typically referred to as an aura) may precede the loss of awareness or consciousness. In some cases, seizures can be lessened by drug, lifestyle and/or surgical intervention. However, some cases of epilepsy are uncontrollable, or “intractable.” Intractable epilepsy is severe and may result in physical harm to the body, compromised quality of life and shortened lifespan. Further, persons with intractable epilepsy may be limited in terms of suitable opportunities for education and employment, which undoubtedly impairs quality of life.
Severe seizures, especially those involving unusual movement or behaviour, can appear to be dramatic and may be frightening to some, adding to the misconception that epilepsy is an unpredictable and violent disorder. Additionally, the stigma associated with epilepsy often means that persons who experience seizures face consequences in daily life above and beyond those which are a direct result of the condition.
Click to download the chart pack or infographic!
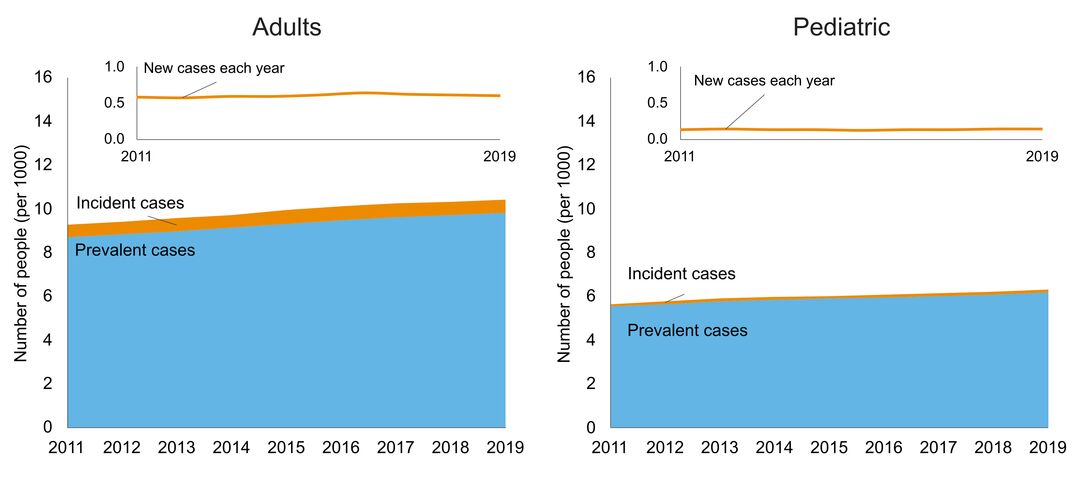
- number of people in Ontario with the disorder
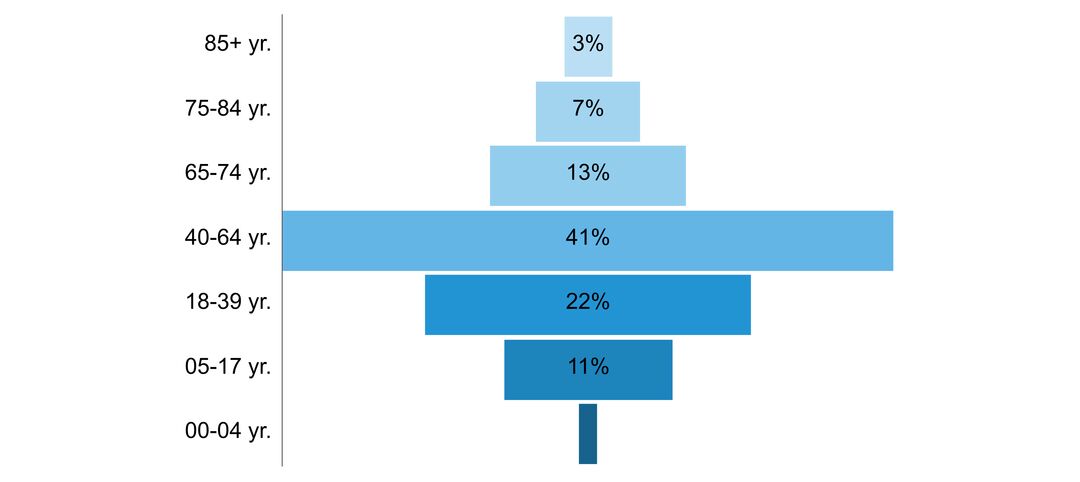
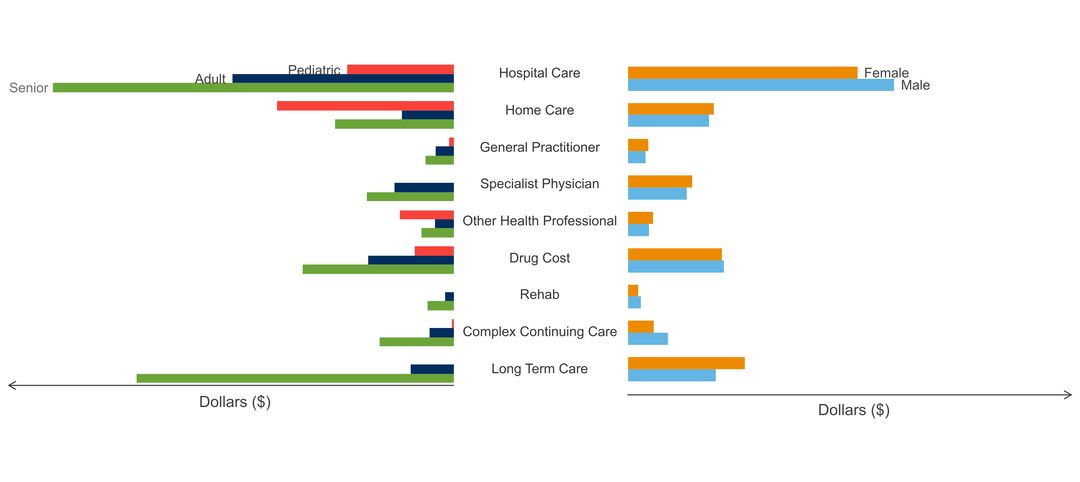
- age of people with the disorder
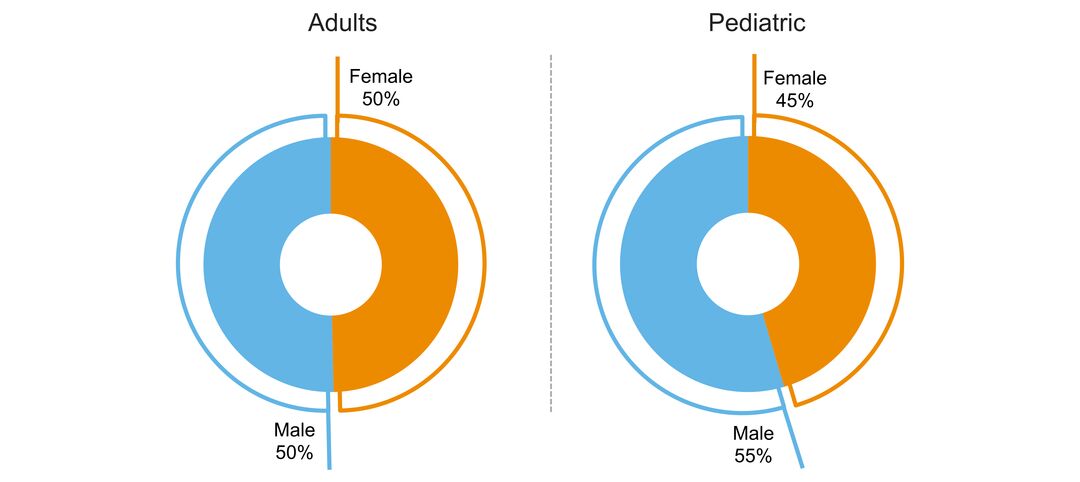
- sex ratio of people with the disorder
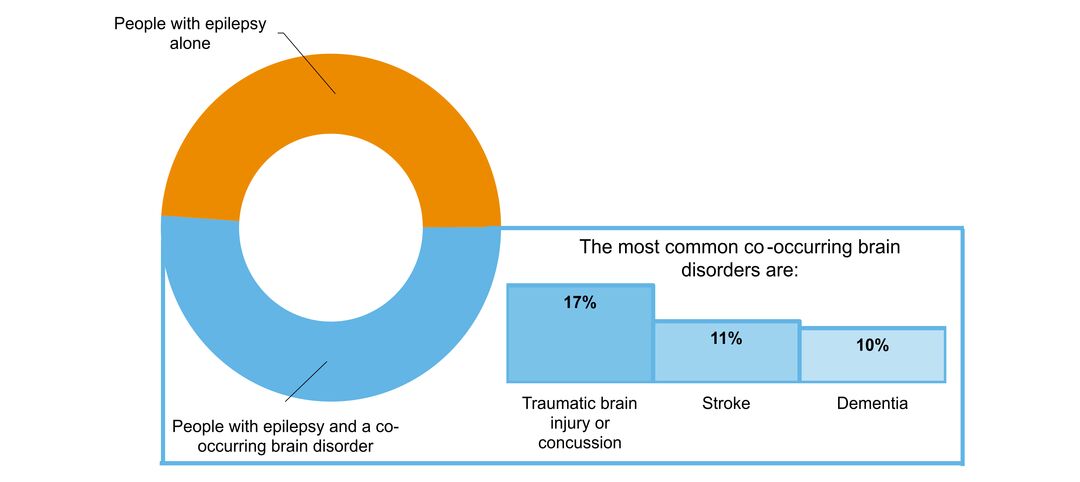
- what other brain disorders commonly co-occur
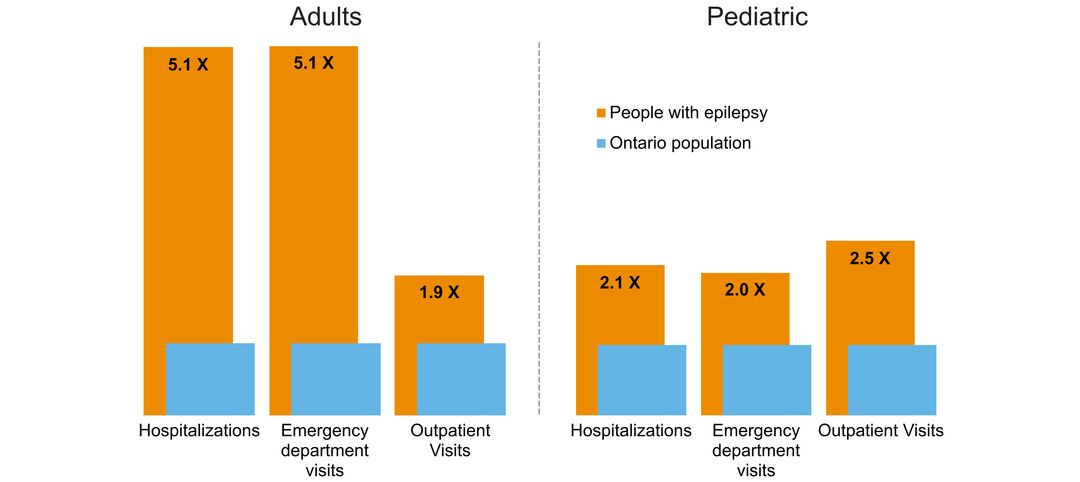
- overlap with mental health and addictions health system use
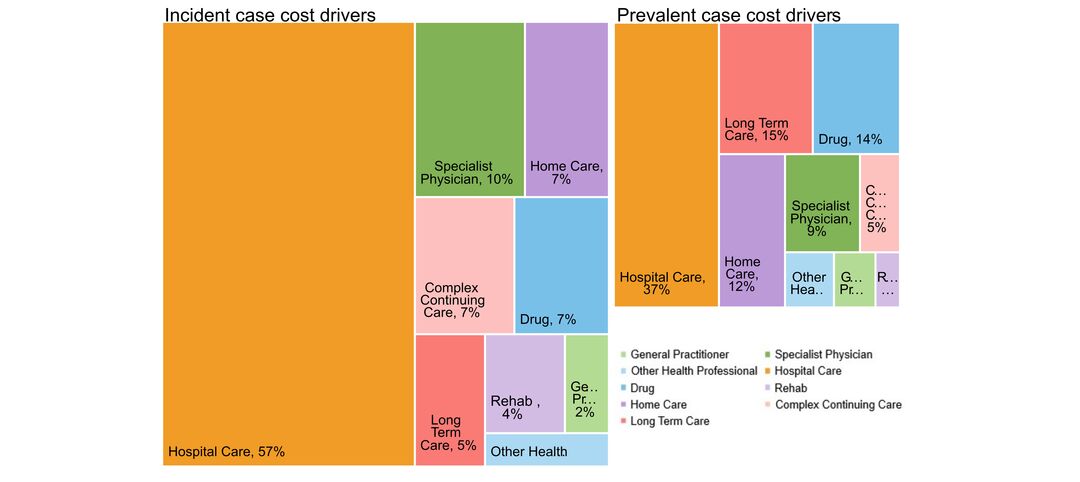
- costs & cost drivers associated with health system use