Dementia
What is it?
Dementia (including Alzheimer’s disease)
As individuals age, they may see a decline in one or more areas of their thinking, such as memory or decision-making. Changes of this nature seen with normal aging are mild and do not have a significant impact on the ability to live independently. However, if the decline interferes with independence in everyday activities and cannot be explained by another mental disorder like a depression or a delirium (acute confusional state), it is characteristic of a disorder called dementia. In addition to its cognitive and functional manifestations, dementia can be associated with changes in mood and behaviour.
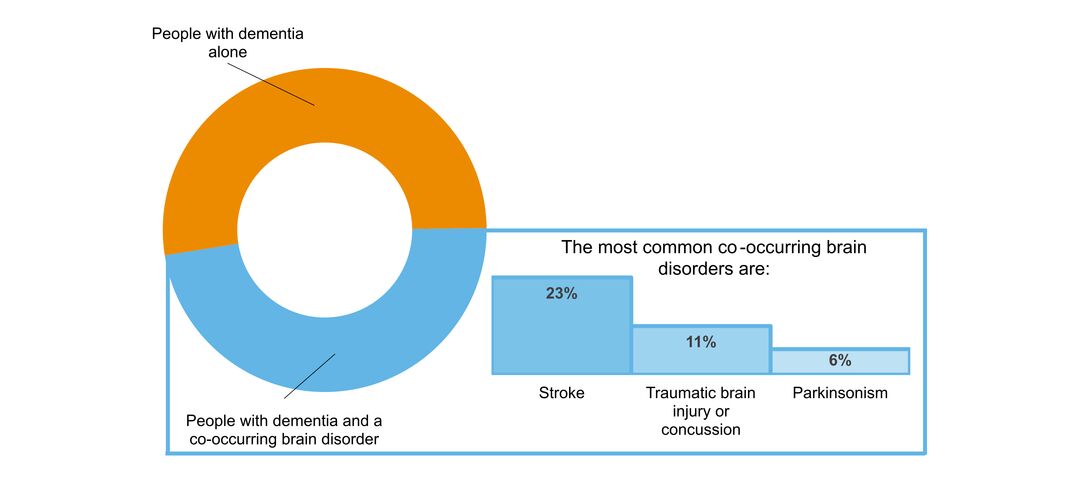
There are many possible causes of dementia. The most common is a condition called Alzheimer's Disease, which accounts for approximately 6 in 10 cases of dementia. Other causes include vascular dementia (where the problem arises from cerebrovascular disease), Parkinson's disease, and Lewy body dementia, fronto-temporal degenerations like Pick’s disease, traumatic brain injuries, and excessive consumption of alcohol. It is not unusual in older persons with a dementia to find more than one underlying cause.
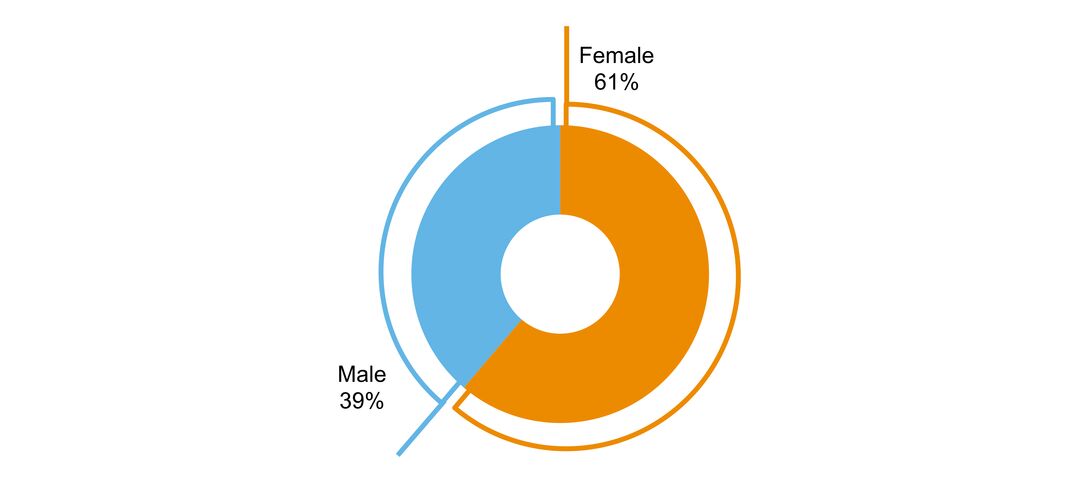
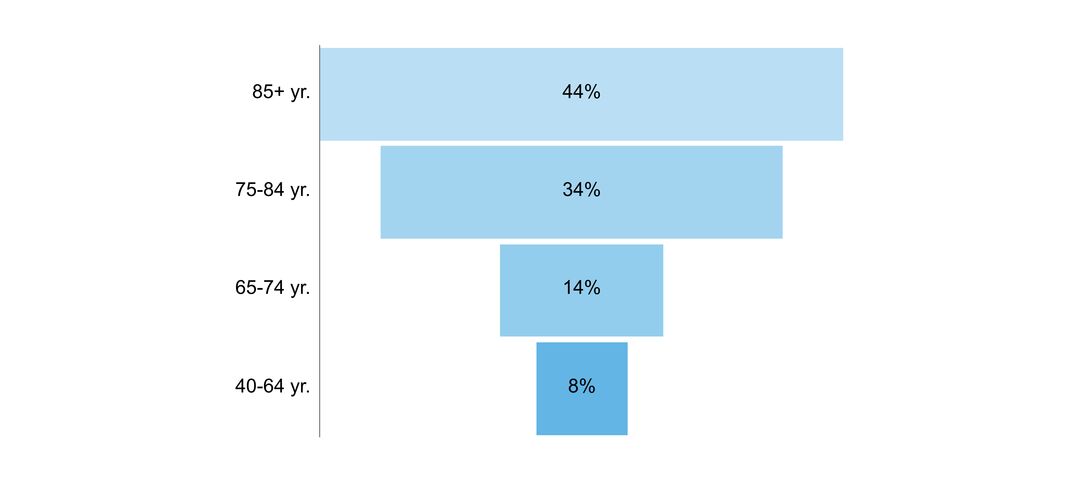
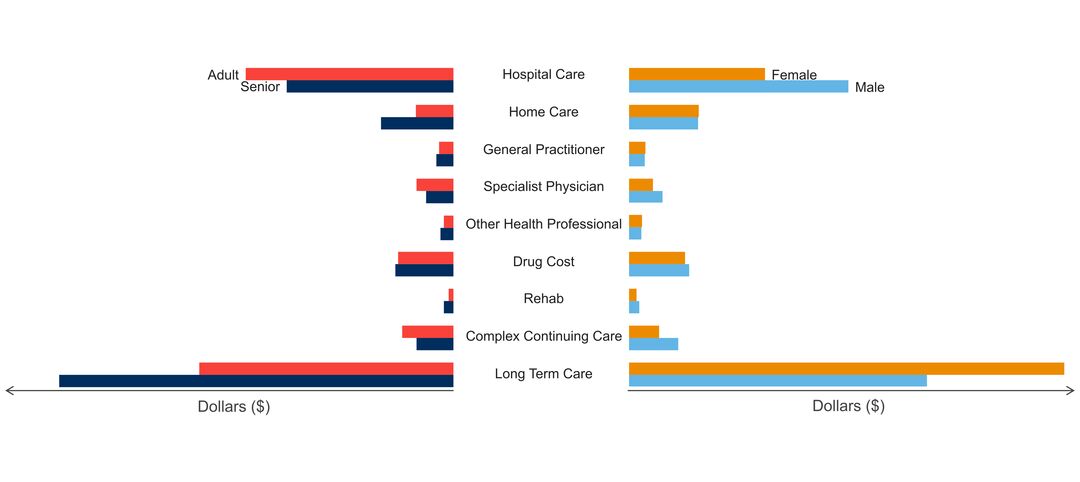
Dementia arises from changes in the structure and function of people’s brains. Although there is a growing understanding of dementia and its causes, there is much to learn. Dementia is more common after the age of 65 and affects both men and women. Primarily because women in general live longer than men, there are more women with dementia.
Doing things like protecting the head from injury, avoiding excessive alcohol intake, following a heart-healthy diet, and living an active physical, mental and social life can decrease a person’s risk of developing a dementia. A healthy lifestyle may ward off dementia just as it does other conditions. Because dementia often progresses over time, it is important to ensure early on that advance planning is done. Options for drug treatment of the more common causes of dementia are limited. The agents currently available for Alzheimer’s disease can provide modest benefits for some of the symptoms of this condition, but these drugs do not prevent progression of the illness, not everyone responds, and side effects can occur. Dementia can have a profound impact on the quality of life of the person with the condition and their primary caregiver, who is often a spouse or other family member. Over time, services typically have to be mobilized to support dementia sufferers, with many of them eventually having to move into a care facility.
Click to download the chart pack or infographic!
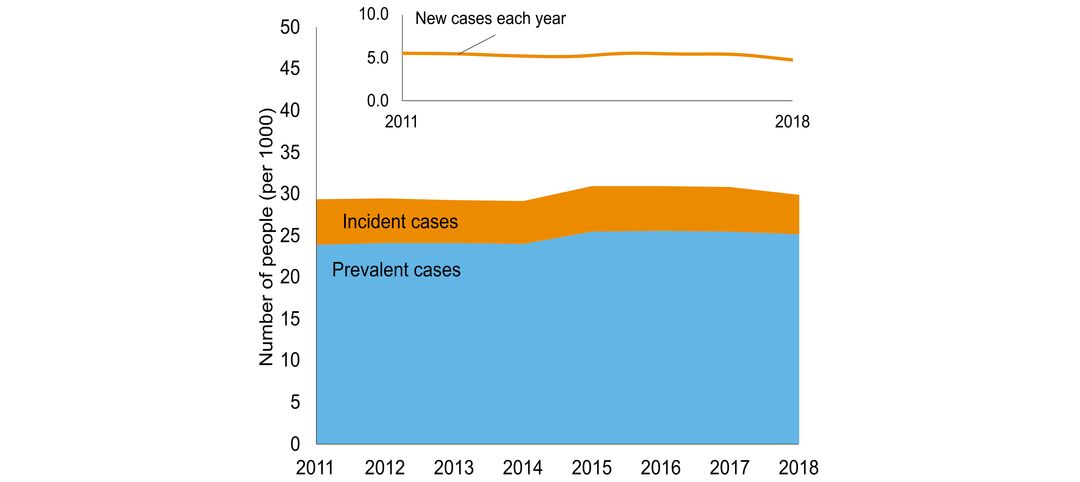
- number of people in Ontario with the disorder
- age of people with the disorder
- sex ratio of people with the disorder
- what other brain disorders commonly co-occur
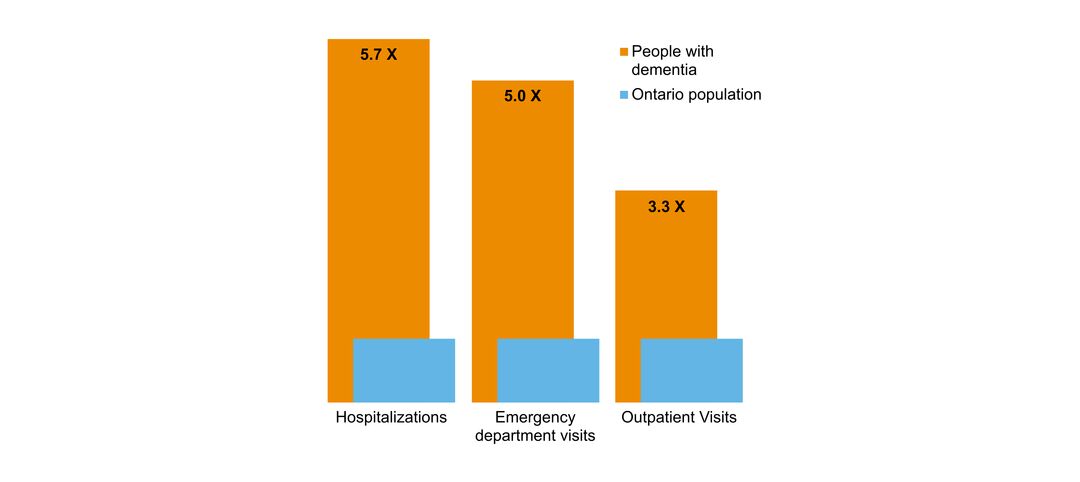
- overlap with mental health and addictions health system use
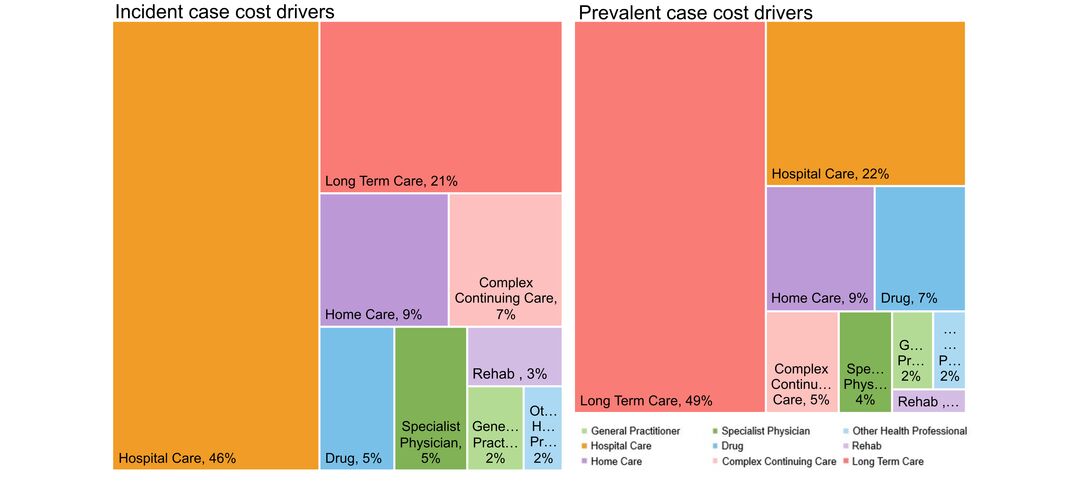
- costs & cost drivers associated with health system use